
Infectious Disease News With Views
Archive - 2013
 U.S. Flu Activity Ticks Up: The Week 50 Update
U.S. Flu Activity Ticks Up: The Week 50 Update
24Dec13
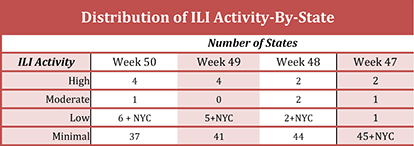
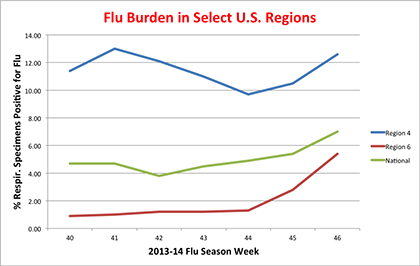
The latest data from the CDC for the week ending December 14th (week 50) has been published. The data shows that flu activity in the U.S. increased significantly over the preceding week (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 17.8% nationally, up from 13.3% the prior week. Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN], 5 [IL, IN, MI, MN, OH, WI], and 6 [AR, LA, NM, OK, TX] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). Region 8 [CO, MT, ND, SD, UT, WY] followed, below the national average at 17.7%, while the remaining regions were below the national average.
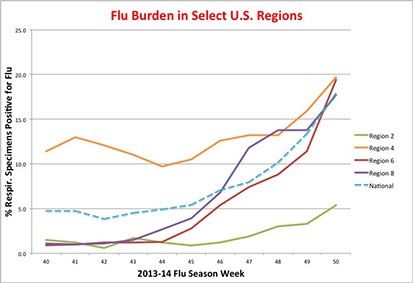
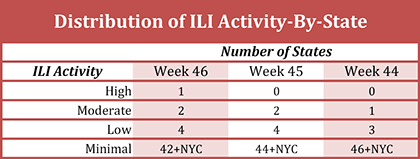
The pneumonia and influenza (P&I) mortality index is 6.6% (6.2% last week), below the epidemic threshold of 6.9% for week 50, and there were two influenza-associated pediatric deaths reported. The proportion of outpatient visits ascribed to influenza (ILI) was 2.3% (versus 2.1% last week), just above the national baseline of 2%. The distribution of ILI activity-by-state now shows four states with “high ILI activity” (see table below). When typed, the majority of isolates were influenza A (~97% of typed specimens) and, while only 45.6% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 97%; roughly 3% were H3N2).
The number of Tamiflu-resistant isolates detected this season remained at 7. By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
 Two More Cases of H7N9 in China’s Guangdong Province
Two More Cases of H7N9 in China’s Guangdong Province
19Dec13 Updated: 20-Dec-13
China’s official news agency, Xinhua, is reporting (here and here) two additional confirmed human H7N9 infections, one on Wednesday and the other today (Thursday), in the southern province of Guangdong. There have now been four new cases reported in the past five days in Guangdong Province.
The case reported on Wednesday (62M) hails from Yangjiang City and is currently in critical condition. In response, the “…province dispatched five inspection teams to 21 cities and a district on Wednesday to strengthen H7N9 prevention and control efforts.”
The second case (38M), a resident of Shenzhen City, displayed initial symptoms of flu on 09Dec13 and received treatment at a local clinic. The patient tested positive for H7N9 on 17Dec13 and the test result confirmed on 18Dec13. “he patient is receiving treatment at the Shenzhen No. 3 People's Hospital and is in critical condition.”
This brings the total number of confirmed H7N9 infections in Guangdong Province this season to 6. The first two patients this season (51F & 3M) have since recovered fully and have been discharged from hospital. According to another report from Xinhua, “”"According to expert assessments, Guangdong faces an extremely high risk of sporadic human H7N9 infections this winter and next spring," said Zhang Yonghui, head of the provincial center for disease control and prevention.”
This cluster of recent cases seems to point towards the Longgang District of Shenzhen City where, on Dec. 11th, three distinct environmental samples from two poultry markets tested positive for the H7N9 strain. The two poultry “wet” markets where positive specimens were obtained (Kangqiao and Henggang) were ordered closed for one week (starting on Dec. 11) for culling of stock and site sterilization; these markets are now presumably open again. There is no direct evidence linking the confirmed human cases of H7N9 infection to these two markets.
However, three of the recent human cases have visited the Longgang District. The 38M patient “…is a migrant worker who lives and works in Nanwan Street, in Longgang district, near one of the infected markets where authorities found the H7N9 virus on December 11.” The recent 39M patient “commuted to the district (Ganlan area)” and the 36F patient from Hong Kong who visited the Longgang District “... is believed to have handled a live chicken at a flat in Nanwan Street before falling ill.” In addition, the second Hong Kong patient (80M) had recently traveled to Shenzhen City, though there was no apparent contact with chickens. Interestingly, the chicken vendor from one of the two suspect “wet” markets “…bought all her live chickens from the Buji Poultry and Livestock Wholesale Market, about three kilometres from the Kangqiao facility.”
So many cases, relatively speaking, with a footprint in the Longgang District provides a valuable clue for epidemiological investigations but also raises concerns of substantial spread of the virus in the local population, even if sub-clinical or asymptomatic in presentation. This is a population-dense region and a significant up-tick in critical case numbers could be a lagging indicator of wide dissemination of the virus.
 A Year of Firsts for Influenza: Flu A/H10N8 Claims Its First Known Human Fatality
A Year of Firsts for Influenza: Flu A/H10N8 Claims Its First Known Human Fatality
18Dec13
It has been an impressive year of “Firsts” for influenza. Among this years list of “first-ever” events are the outbreak of A/H7N9 that began last spring and continues even now. There was also the first-ever reported case of human infection by A/H6N1, which occurred earlier this year in Taiwan. Now comes news of the first ever case of a human fatality due to influenza A/H10N8 Infection (see press reports here and here, as well as remarks from the WHO).
The patient (73F) lived in Jiangxi Province and passed away on 06Dec13 from respiratory failure. Her symptoms included severe pneumonia, respiratory distress, high blood pressure, as well as a neuromuscular disorder. The patient had a variety of underlying medical conditions (i.e. patient was immuno-compromised).
The source of the infection is unknown. The patient had been to a live bird market four days prior to the onset of symptoms. Influenza A/H10N8 is considered a low pathogenicity avian influenza virus most prevalent in aquatic waterfowl.
Just last year, a team from the College of Veterinary Medicine, South China Agricultural University and the Guangzhou Animal Health Inspection Institute reported [ http://jvi.asm.org/content/86/14/7716.full ] a complete genomic sequence on a A/H10N8 isolate obtained, for the first time, from a live bird market (duck)in Guangdong Province.
Why is this a concern and not just an oddity detected by chance due to enhanced flu surveillance in China? Part of the answer can be found in a paper published in 2011 which studied an H10N8 isolate from the Dongting Lake wetland reservoir, an important site for East Asian migratory birds. The results in the paper showed that while the virus was only of low pathogenicity for chickens, it replicated efficiently in the mouse lung without prior adaptation, and the virulence to mice increased rapidly during adaptation in mouse lung. Indeed, the virus became lethal after only two passages in the lung. Such observations suggest a low barrier for some LPAIs to become mammalian pathogens of high pathogenicity.
As noted by these investigators, an earlier study had demonstrated direct transmission of an influenza A virus directly from wild birds to humans, in this case “…influenza A/H11 infection in persons who were routinely, heavily exposed to wild ducks and geese through recreational activities (duck hunting) or through their employment (bird banding).” In the realm of domestic birds, direct H7N7 infection of humans can lead to mild illnesses, such as conjunctivitis, and even to more serious disease (see here). Of particular note is the finding from the H11N9 study group of a “…relative lack of antibody response in our study population, who had substantial exposures to waterfowl with influenza A infections, and in inoculated volunteers from Beare and Webster (12) suggests that avian influenza infections in humans exposed to wild waterfowl may occur more commonly than we are able to detect with current methods.” Induction of mere low antibody responses, if coupled to high rates of adaptation to mammalian hosts with high pathogenicity characteristics, is a worrisome combination for human health.
 Welcome to the Americas, Chikungunya!
Welcome to the Americas, Chikungunya!
18Dec13
The first-ever documented case of “local” chikungunya virus infection in humans in the Americas has been reported on the Caribbean island St. Martin according to a ProMED email. “As of 10 Dec 2013, altogether, 2 confirmed, 4 probable, and 20 suspected cases of chikungunya [virus] infection have been reported.” A more recent news report states that the number of confirmed cases is now “about a dozen” with “dozens more” suspected cases. The WHO and the U.S. CDC are both citing ten confirmed cases on the island. The U.S. CDC has issued an alert (Watch Level 1) for those traveling to St. Martin.
According to the CDC, “A total of 109 laboratory-confirmed cases of chikungunya were identified in the United States from 1995 through 2009. All were in travelers, and all but three of them occurred between 2006 and 2009 when there were large outbreaks of the disease ongoing in India and Indian Ocean Islands. From 2006 through 2009, an average of 26 travel-related chikungunya cases was identified per year.” Globally, chikungunya has re-emerged in 2004, after years of chemical spraying directed at its mosquito host, and has spread to new locations across the globe, including Europe. Annually, there are millions of cases in countries across the globe, but especially around the Indian Ocean.
Chikungunya is an acute febrile viral disease that is rarely fatal. Patients usually present with the onset of high fever, severe joint pain, and rash. The disease was first identified in Africa in the 1950’s on the Makonde Plateau. The name chikungunya is derived from the Makonde verb kungunyala, refering to “that which bends up”; patients with long-term joint pain in the lower extremities develop a stooped gait. Infection with chikungunya virus is rarely fatal but the joint pain (polyarthralgias) seen with chikungunya can often be severe and debilitating. There is currently neither vaccine nor therapeutic agent for the infection. Patients recover in about a week, although long-term joint pain occurs in some people.
The virus does not spread person to person. Like its closely related viral cousin, dengue, the virus is spread by mosquitoes, notably Aedes aegypti and Aedes albopictus. Both of these strains are seeping into the U.S. and this past season saw a number of dengue cases in the U.S., especially in Florida and Texas. As these mosquito vectors gain a better foothold in the U.S., the number of cases of mosquito-born viral diseases, such as dengue and chikungunya, are expected to grow.
 Two New H7N9 Case in China’s Guangdong Province
Two New H7N9 Case in China’s Guangdong Province
15Dec13 Updated: 16-Dec-13
A news story from China’s official news agency Xinhua reports the occurrence of another confirmed case of human H7N9 infection, this time in China’s southern Guangdong Province. The patient (39M) is a resident of Dongguan City and is hospitalized in serious condition.
This is the second confirmed case of human H7N9 infection this fall season, the prior case (3M), also a resident of Dongguan City, was reported on Nov. 5th. A total of 53 close contacts of the most recent patient have been identified but without any indication of influenza infection so far.
Update of Dec 16th: Xinhua is reporting a second confirmed case of human H7N9 infection this week. The patient (65F) is from Yangjiang in Guangdong Province and is in serious condition.
These reports come on the heel of news late last week of health officials in Shenzhen City (also in Guangdong Province) closing two live poultry markets in the Longgang District for one week following the detection of H7N9 virus in avian specimens. Nearby Hong Kong has recently reported two confirmed human cases of H7N9 influenza this fall as well.
This brings the global total of confirmed H7N9 infections in humans to 145 and this season's total to 10: 5 in the southern region of Guangdong Province and Hong Kong and 5 in the northern region of Zhejiang Province. As repeatedly noted by Recombinomics (see here for example), sequences from these two regions are similar but distinct. Specifically, the published sequence from one of the Hong Kong cases shows characteristics in internal genes known to be circulating in H9N2 infected poultry in southern China. In parallel, recently released sequences from Zhejiang Province had internal gene sequences reflecting characteristics of H9N2 circulating in poultry in northern China. This dichotomy reflects the ongoing evolution of the H7N9 virus and will require careful monitoring as the current season progresses.
 WHO Confirms 2 More H7N9 Cases: One the 2nd in HK
WHO Confirms 2 More H7N9 Cases: One the 2nd in HK
11Dec13
In a Global Alert and Response (GAR) issued yesterday, the WHO confirmed two additional cases of human H7N9 infection: one in China’s Zhejiang Province and the other in Hong Kong. This brings the total number of new H7N9 cases this flu season to eight: 2 in Hong Kong and 6 in China. For a summary of the latest human H7N9 cases, please see this web page).
The new case in Zhejiang Province is “…a 30-year-old man from Zhejiang Province. He became ill on 29 November 2013 and was admitted to hospital on 5 December 2013. He is currently in critical condition.” This patient is also the son-in-law of the 57M patient from Zhejiang Province reported just last week (for an updated listing of H7N9 patients to date, please see the this web page). It has yet to be confirmed that this patient was infected via contact from his father-in-law, though the timing of their infections is suspicious. According to a report on China’s Xinhua web site, “We can’t rule out the possibility that the father transmitted the virus to his son in law, because they were not living together before the father caught bird flu. But after the father was sick, the son was looking after him.” Li Lanjuan, director of Infectious Diseases Lab, said.”
In Hong Kong, a second H7N9 patient (80M) has been identified. This patient is not linked to Hong Kong’s first H7N9 patient, reported last week. Rather, he is a resident of Shenzhen City and has an underlying medical condition for which he travels to Hong Kong for treatment. The patient “…was admitted to a hospital in China, Hong Kong SAR, on 3 December 2013. He was afebrile on admission and developed fever on 6 December 2013.” Meanwhile, news reports today (see here and here) cite evidence of H7N9 being detected in two Shenzhen poultry markets. Specifically, “…three out of 70 environmental samples collected from 13 wet markets had tested positive for the deadly bird flu strain. The samples were collected from chicken stools, cutting boards and depilators collected from live chicken stalls at two wet markets in the city’s Longgang district.”
Finally, a new study published yesterday in Nature Communications by investigators from New York’s Mount Sinai School of Medicine found that Tamiflu-resistant H7N9 retains its ability to replicate in human cells and cause severe disease. That is, this virus can obtain genetic alterations conveying drug-resistance with out the usual impact to its “fitness” as a human pathogen. The study notes that these observations on A/H7N9 are in contrast to what was observed with the A/H3N2 influenza subtype. The authors hypothesize that “…maintenance of virus fitness is enabled, at least in part, by concurrent, compensatory changes in the expression of HA. The development of oseltamivir resistance, unaccompanied by demonstrable losses of replicative ability in vitro or of virulence or transmissibility in vivo, underscores the multigenic and sometimes unpredictable nature of fitness in influenza A viruses.”
 U.S. Seasonal Flu Activity: Week 48 Data
U.S. Seasonal Flu Activity: Week 48 Data
10Dec13
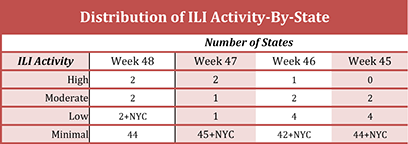
The latest influenza data from the CDC for the week ending November 30th (week 48) has been published. The data shows, generally, that levels of flu activity in the U.S. increased slightly over the preceding week (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 10.1% nationally, up from 7.9% the prior week. Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN], 5 [IL, IN, MI, MN, OH, WI], and 8 [CO, MT, ND, SD, UT, WY] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). Region 6 [AR, LA, NM, OK, TX] followed, just below the national average at 8.8%, while the remaining regions were well below the national average.
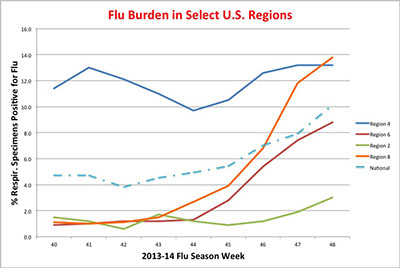
The pneumonia and influenza (P&I) mortality index is 5.8%, below the epidemic threshold of 6.6% for week 48, and one influenza-associated (A/H1N1p09) pediatric death was reported. Similarly the proportion of outpatient visits ascribed to influenza (ILI) was 1.9% (versus 1.7% last week), below the national baseline of 2%. The distribution of ILI activity-by-state now shows two states with “high ILI activity” (see table below). When typed, the majority of isolates were influenza A (~94% of typed specimens) and, while only 45% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (nearly 96%; roughly 4% were H3N2).
The number of Tamiflu-resistant isolates detected this season remained at 6. By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
 Global MERS-CoV Count Climbs to 163
Global MERS-CoV Count Climbs to 163
02Dec13
The WHO issued an update today on the SARS-like novel corona virus (MERS-CoV). A major focus of the report is the recent cluster of three laboratory-confirmed cases of MERS-CoV in the United Arab Emirates (UAE).
"The three cases belong to a family in Abu Dhabi – a mother (32 years old), father (38 years old) and son (8 years old). The earliest onset of illness was 15 November 2013. Both the mother and father are in a critical condition in hospital. They had no travel history, no contact with a known confirmed case and no history of contact with animals. While hospitalized, the mother gave birth to a newborn child. The 8 year old son, who has mild respiratory symptoms, was detected from epidemiological investigation of family contacts, and is being kept in hospital isolation."
With these latest cases, the global count of lab-confirmed MERS-CoV cases has increased to 163 with 70 deaths. However, media reports out today (see here and here) indicate that while the mother had delivered her child by emergency C-section yesterday, she has since expired. Recombinomics has raised concerns that this familial cluster and other recent cases all traveled through the Kingdom of Saudi Arabia (KSA) following the recent Hajj and are indicative of the increasing export of MERS-CoV from the KSA.
 Another Case in China of Human Infection by Flu A/H7N9
Another Case in China of Human Infection by Flu A/H7N9
30Nov13
Another case of human infection by influenza A/H7N9 has been reported by the official Chinese News Agency, Xinhua. This marks the fifth case of H7N9 influenza reported this fall and the third in November. Nonetheless, it is still too early to tell if there will be another signiificant "wave" of human influenza cases due to H7N9, although China's CDC warning about such a possibility remains in place.
The latest case involves a 57M patient from Zhejiang Province who tested positive for the virus on Nov. 27th when he went to a hospital complaining of a fever. The patient subsequently "... suffered respiratory failure and shock and is still in critical condition..."
This latest cases bring the global count of confirmed human infections by flu A/H7N9 to 140 with 45 deaths. All known cases occurred this year. Four of the five cases reported this fall, all in China, hail from Zhejiang Province.
 Confirmed: The 2009 H1N1p Flu Pandemic Worse than Thought
Confirmed: The 2009 H1N1p Flu Pandemic Worse than Thought
29Nov13
Additional confirmation has been obtained that the pandemic influenza outbreak of 2009 was worse than originally painted and markedly worse in select geographical regions such as the Americas. This pandemic was caused by the appearance of a new flu virus, H1N1pdm09, in the spring of 2009. The H1N1pdm09 virus is a distant cousin to the H1N1 flu virus that caused the great "Spanish Flu" pandemic in 1918-1920.
In a new study just published in the journal PLoS Medicine, investigators from the WHO found that roughly 203,000 people died globally during the period 01April09-31Dec09. This is a much higher fatality count than the official figure of 18,631 lab-confirmed fatalities tallied by the WHO for the period 01Mar09-10Aug10. While it is generally understood that the "true" mortality burden associated with an epidemic or pandemic outbreak is always higher than that suggested by the number of deaths among lab-confirmed patients, the "true" level of the burden is often poorly understood.
To obtain a better understanding of the true mortality burden of the 2009 swine flu pandemic, investigators from the WHO's Global Pandemic Mortality [GLaMOR] project accrued data from 20 countries (representing 1/3 of the global population) to derive cause-of-death time series over the time period 2005–2009. They then employed a multivariate linear regression model to measure the numbers and rates of pandemic influenza respiratory deaths in each of these countries and then used a second statistical modeling tool to extrapolate globally from the 20 single country values.
Two additional findings are of particular note. First, the vast majority of fatalities during the pandemic period were in the population less than 65 years of age, in stark contrast to a "typical" seasonal flu season where the vast majority of fatalities occur in the population greater than 65 years of age. Second, there were stark geographic differences in mortality rates due to H1N1pdm09. For example, certain countries in South and Central America had mortality rates 20 times greater than those observed in Europe.
The present study does have limitations that qualify its results. First, the lack of data from low income countries likely attenuates final global estimates since poverty and malnutrition provides fertile grounds for influenza. Second, the data set used likely underestimates the mortality burden due in the 20 included countries (missing deaths due to flu late in 2009 and all through 2010; only flu-related deaths that were recorded as respiratory deaths were included).
Nonetheless, these results are congruent with results published last year in a study by the CDC. This earlier study estimated the global mortality burden for the pandemic at between 151,700 and 575,400 deaths and that a "...disproportionate number of deaths occurred in Southeast Asia and Africa, where access to prevention and treatment resources are more likely to be limited."
Hopefully, confirmation of a much higher mortality rate during the pandemic will go a long way in mitigating the criticism heaped on the WHO for its response to the outbreak.
 Another H5N1 Death in Indonesia
Another H5N1 Death in Indonesia
24Nov13
The number of laboratory-confirmed cases of human H5N1 infection this year in Indonesia that resulted in mortality reportedly increased last week with the death of a 31F patient in Bekasi Timur, a district east of Jakarta. A total of three H5N1 patients have died this year in Indonesia. This places Indonesia, along with China and Egypt, second only to Cambodia in H5N1 deaths this year. To date, 641 lab-confirmed cases of H5N1 have been reported globally since 2004 including 380 deaths.
 Cambodian Cases of Human H5N1 Infection Climb to 26
Cambodian Cases of Human H5N1 Infection Climb to 26
14Nov13
The number of laboratory-confirmed cases of human H5N1 infection this year in Cambodia has jumped to 26 with 3 newly reported cases in the past week, according to a news report from the Associated Press (here). Fourteen of these patients have died. The WHO has yet to officially confirm the 25th and 26th cases, having last confirmed the 24th case late last week (here). However, the Ministry of Health for the Kingdom of Cambodia has confirmed the latest cases on their website (here). It remains unclear why Cambodia has been afflicted with so many cases this year.
 Global MERS-CoV Count Climbs to 153 & Spreads Its Reach
Global MERS-CoV Count Climbs to 153 & Spreads Its Reach
13Nov13
The official case count for the novel SARS-like corona virus, MERS, continues growing, as does the associated mortality and geographic spread. According to the CDC's webpage, the global case count now stands at 153 with 64 deaths. Even today, additional cases have been reported in the media, as well as additional deaths. Importantly, two more countries have reported their 1st cases of human MERS infection: Spain and Kuwait. Oman reported its first case last month. This increases the number of countries reporting human cases of MERS infection to 11, though the vast majority of cases (127 with 53 deaths) have been reported in the Kingdom of Saudi Arabia (KSA).
In a related matter, an article appearing today at the website of The Lancet Infectious Disease (here) reports that many symptomatic cases of MERS-CoV infection go undetected, as much as 62% of all cases. The good news is that this may mean that the associated case fatality rate for MERS-CoV infection is substantially over-estimated when considering only confirmed cases. In addition, the authors estimate the reproduction number, R [the number of secondary cases generated by one case, on average, over the course of an infection], in the absence of effective infection control to be roughly 1 ("in the range 0·8—1·3") and giving rise to a slowly growing epidemic either in human beings or in an animal reservoir.
An important step was taken this past week in identifying at least one possible animal reservoir for MERS: camels (see here and here). In brief, a MERS patient in KSA owns a pet camel, also ill, that tested positive by PCR for MERS-CoV. As noted in the New York Times article, this is the latest observation in support of a link between MERS-CoV in camels and human infection. "In three earlier clusters of MERS cases, the first patient to fall ill in each was reported to have had contact with a sick camel. Although antibodies to the disease had been found in camels before, the virus itself had not." Perhaps now it has. Investigators at the Ministry of Health in KSA are working to obtain full sequences of the virus, from both the human case and the pet camel, to confirm identity of the infecting virus in both. As always, if viral identity is found in both the patient and the camel, even more questions will be raised, such as: 1) how does human infection actually occur? and 2) are there many low-grade or even asymptomatic human infections that go undetected since the virus may be widespread in camels (based on detection of MERS-CoV binding antibodies in various camel populations; see here)? But first, we must await the sequencing data from this patient and his pet camel.
Finally, an excellent overview of the first 144 laboratory-confirmed cases of MERS-CoV infection (from Sept 2012 thru Oct. 2013) has just been published in PLoS Current Outbreaks (here) and is worth a good read.
 U.S. Flu Activity Ticks Up: The Week 49 Update
U.S. Flu Activity Ticks Up: The Week 49 Update
14Dec13
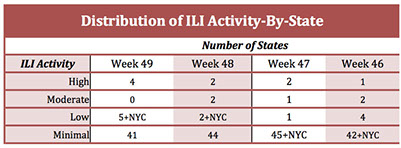
The latest data from the CDC for the week ending December 7th (week 49) has been published. The data shows that flu activity in the U.S. increased significantly over the preceding week (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 13.3% nationally, up from 10.1% the prior week. Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN], 5 [IL, IN, MI, MN, OH, WI], and 8 [CO, MT, ND, SD, UT, WY] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). Region 6 [AR, LA, NM, OK, TX] followed, below the national average at 11.4%, while the remaining regions were well below the national average.
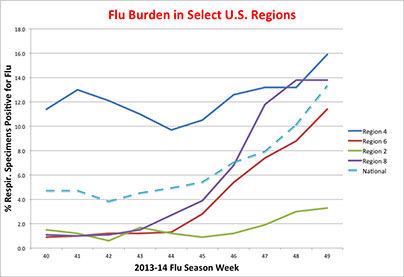
The pneumonia and influenza (P&I) mortality index is 6.2%, below the epidemic threshold of 6.8% for week 49, while no influenza-associated pediatric deaths were reported. The proportion of outpatient visits ascribed to influenza (ILI) was 2.1% (versus 1.9% last week), just above the national baseline of 2% for the first time this season. The distribution of ILI activity-by-state now shows four states with “high ILI activity” (see table below). When typed, the majority of isolates were influenza A (~94% of typed specimens) and, while only 50% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 96%; roughly 4% were H3N2).
The number of Tamiflu-resistant isolates detected this season increased by one to 7. By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
 U.S. Seasonal Flu Activity: Week 47 Data
U.S. Seasonal Flu Activity: Week 47 Data
03Dec13
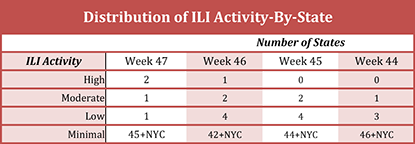
The latest influenza data from the CDC for the week ending November 23rd (week 47) has been published. The data shows, generally, that levels of flu activity in the U.S. remain low, though slightly increased over the preceding week (for a graphical round-up of the data, please see here) . The percentage of respiratory specimens testing positive for influenza increased to 7.9% nationally, up from 7% the prior week. Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN] and 8 [CO, MT, ND, SD, UT, WY] led the pack with a % of specimens positive for flu in excess of 10% (see graph, below). Regions 5 [IL, IN, MI, MN, OH, WI] and 6 [AR, LA, NM, OK, TX] followed, just below the national average, while the remaining regions were well below the national average.
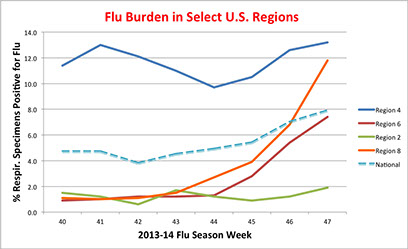
The pneumonia and influenza (P&I) mortality index is 5.8%, below the epidemic threshold of 6.6% for week 47, and no influenza associated pediatric deaths were reported. Similarly the proportion of outpatient visits ascribed to influenza (ILI) was 1.7% (versus 1.5% last week), below the national baseline of 2%. The distribution of ILI activity-by-state now shows two states with “high ILI activity” (see table below). When typed, the majority of isolates were influenza A (~88% of typed specimens) and, while only 64% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (nearly 95%; roughly 5% were H3N2).
Interestingly, the CDC reported 2 additional instances of oseltamivir (Tamiflu) resistance for Wk 47. This brings to 6 the number of Tamiflu-resistant isolates detected this season: two in Wk 44, one in Wk 45, and one in Wk 46. In comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
 Hong Kong Reports First Human Case of Flu A/H7N9
Hong Kong Reports First Human Case of Flu A/H7N9
02Dec13
Hong Kong today confirmed its first reported case of human infection by influenza A/H7N9 (see reports here, here, and here). This marks the 6th confirmed case of H7N9 this Fall, globally.
The 36F patient is an Indonesian domestic helper employed by a Hong Kong family of four. The patient was in Shenzhen, China (a major city in southern Guangdong Province, just north of Hong Kong, reportedly in contact with poultry) last month and fell ill on 21Nov13, was admitted to Tuen Mun Hospital on 27Nov13, and finally transferred to Queen Mary Hospital on 30Nov13. The patient is currently in critical condition with severe pneumonia and breathing with the help of an "artificial lung". The patient's close contacts "...have minor symptoms and are being isolated in Princess Margaret Hospital."
In addition, the following points are worth noting:
1. Hong Kong has raised its response level from 'alert' to 'serious' under its preparedness plan for influenza pandemic.
2. The Government is seeking a traveling companion of the patient who also made the trip to Shenzhen last month.
3. Two earlier tests for the virus were negative but a third test yesterday confirmed the presence of H7N9.
While the first occurrence of a contagious disease in a major metropolitan area is always of concern, it is too early to ascribe this event to anything other than a singular, "imported" event. Nonetheless, it is clear that the H7N9 virus has continued to spread into new geographical regions. There have been no confirmed cases of H7N9 flu in Shenzhen to date, though there was one recent case (3M) in mid-October in nearby Dongguan City, also in Guangdong Province. Curiously, both this case and the recent Guangdong case describe close contacts ill with minor flu-like symptoms, a rare event in cases earlier this year in China.
 Dengue in U.S., Fall 2013
Dengue in U.S., Fall 2013
30Nov13
A spate of dengue cases has appeared this fall in the U.S., according to a report from CIDRAP News. In Long Island's Suffolk County, the first-ever locally acquired (in a patient who has not recently traveled to a dengue endemic region and therefore has been bitten by a local, infected mosquito) dengue infection in New York State was reported on the 20th of November. ""Given the recent introduction of Aedes albopictus [mosquitoes] into New York State and the high level of travel in New York to areas of the world endemic for dengue, it is not surprising that a locally acquired case of dengue has been found in the state," said State Health Commissioner Nirav R. Shah, MD, MPH."
Texas is also experiencing a number of dengue cases. According to a recent news story, 32 cases had been reported in the Rio Grande Valley as of 21Nov13, though only a fraction of these may be locally acquired.
According to the Nov. 23 update from Florida Health, "In 2013, a total of 23 cases of locally acquired dengue have been reported in 21 Florida residents and two out-of-state-residents. Exposures occurred in two counties, Martin (22) or Miami-Dade (1)." The same update notes that 180 cases of imported dengue have been reported this year.
By way of comparison, it should be noted that, as of 19Nov13, 7,221 cases of locally-acquired dengue occurred in Puerto Rico this year.
The rapidly changing prevalence of local dengue cases reflects new geographic spread of Aedes albopictus mosquitoes in the US.
 U.S. Seasonal Flu Activity: Low But Stirring
U.S. Seasonal Flu Activity: Low But Stirring
23Nov13 Updated 25Nov13
The latest data from the CDC for the week ending November 16 (week 46) shows that levels of flu activity in the U.S. remain low, though signs of increasing activity are present (see data summary here). The percentage of respiratory specimens testing positive for influenza increased to 7% nationally, up from 5.4% the prior week. Once again, region 4 [AL, FL, GA, KY, MS, NC, SC, TN] led the pack with a % of specimens positive for flu in excess of 10% (see graph, below). Regions 6 [AR, LA, NM, OK, TX] and 8 [CO, MT, ND, SD, UT, WY] followed, though below the national average.
The pneumonia and influenza (P&I) mortality index is 5.8%, below the epidemic threshold of 6.5% for week 46, and no influenza associated pediatric deaths were reported. Similarly the proportion of outpatient visits ascribed to influenza (ILI) was 1.5%, again below the national baseline of 2%. The distribution of ILI activity-by-state reflected the first report of “high ILI activity” this season, for MS (see table below). When typed, the majority of isolates were influenza A (~90% of typed specimens) and, while only 47% of influenza A specimens were subtyped, the majority of these were identified as 2009 H1N1p (nearly 90%; roughly 10% were H3N2).
Interestingly, the CDC reported yet another case of oseltamivir (Tamiflu) resistance detected for Wk 46. This brings to 4 the number of Tamiflu-resistant isolates detected this season: two in Wk 44, one in Wk 45, and one this week. By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season. As noted by Recombinomics, the CDC has released two sequences from the current flu season that contain the H274Y Tamiflu-resistance mutation in the viral neuraminidase. Both sequences derived from isolates from Louisiana and are likely the two Wk 44 samples. As noted by the CDC, “High levels of resistance to the adamantanes (amantadine and rimantadine) persist among 2009 influenza A (H1N1) and A (H3N2) viruses (the adamantanes are not effective against influenza B viruses).” If either of these influenza strains were to additional become resistant to Tamiflu, as did the distant relative virus to 2009 H1N1p, the seasonal H1N1, then potential therapeutic responses to the viruses would be eroded to a single antiviral, Zanamivir.
The very utility of neuraminidase inhibitors for the treatment of influenza patients is the focus of two recent articles appearing in the journal Pediatrics. In the first of these, investigators from the CDC retrospectively examined influenza-associated pediatric deaths in the U.S. using data accumulated since 2004 (when pediatric influenza-associated deaths became a notifiable event). "The potential for severe outcomes from influenza should be recognized in all children, both those with conditions that place them at higher risk of influenza-associated complications as well as healthy children. The findings of this national surveillance system report highlight the importance of ... early empirical antiviral treatment of all children with suspected or confirmed influenza virus infection who are hospitalized; who have severe, complicated, or progressive illness; or who are at higher risk of influenza-associated complications due to younger age (<2 years) or medical conditions." The authors note that, despite the recommended empirical use of antivirals in children hospitalized due to suspected influenza by the American Academy of Pediatrics' Committee on Infectious Diseases, actual use of antivirals spiked at 77% of such patients during the 2009 H1N1 pandemic but rapidly fell off to 56% of children hospitalized for influenza during the 2010-11 season.
Echoing these finding, a second report appeared online today (Nov. 25th) summarizing a retrospective outcomes study from the California Department of Public Health & the CDC of 784 "...patients aged 0 to 17 years hospitalized in ICUs with laboratory-confirmed influenza from April 3, 2009, through September 30, 2012." Here, "Ninety percent (532 of 591) of cases during the 2009 H1N1 pandemic (April 3, 2009–August 31, 2010) received NAI treatment compared with 63% (121 of 193) of cases in the postpandemic period (September 1, 2010–September 30, 2012; P < .0001)." The authors conclude that "Prompt treatment with NAIs may improve survival of children critically ill with influenza."
Why the fall off of antiviral use in these patients? Clear answers are not at hand. As noted in a blog posted today on the New York Times by Catherine Saint Louis, multiple reasons may be at play including a lessened sense of urgency in the post-pandemic period or physicians unconvinced by the data. Regardless, the utility of neuraminidase inhibitors may be short lived. Careful attention is called for in monitoring the prevalence of neuraminidase inhibitor resistance in clinical isolates of the current season. In recent years, other influenza A types have rapidly gained widespread anti-viral resistance and the -potential exists to lose one of the few remaining arrows in the quiver.
 More Info on First-Ever Human Infection by Influenza/A H6N1
More Info on First-Ever Human Infection by Influenza/A H6N1
14Nov13
This past Spring marked the first-ever confirmed report of human infection by an H6 influenza/A virus. Now, additional information has been published in Lancet Respiratory Medicine (here) on the Taiwanese patient. Importantly, the authors note that the circulating H6N1 virus has "...a G228S substitution in the haemagglutinin protein that might increase its affinity for the human α2-6 linked sialic acid receptor." A media report analyzes the publication in detail here.
 H7N9: Two New Human Cases in China
H7N9: Two New Human Cases in China
06Nov13
The WHO has issued a Global Alert & Response (GAR) notice (here) describing two new cases of human H7N9 infection. This brings the number of new H7N9 infections for the 2013-14 Northern Hemisphere flu season to four (see latest data summary, here).
The first patient (3M) is from southern China’s Guangdong Province and became ill on 29Oct13, was admitted to a local hospital on 31Oct13, and transferred to another hospital on 04Nov13 after routine monitoring of flu-like cases in Changping Hospital indicated the presence of H7N9, according to a news story appearing online at the Xinhua website. He is currently in a stable condition. The patient’s symptoms are very mild (with no fever) and the patient is currently in isolation at the People’s Hospital of Dongguan City. A total of 7 people in close contact with the patient are under observation: three have shown flu-like symptoms though all seven have tested negative for the H7N9 virus. Cases in Guangdong Province are intrinsically noteworthy due to the province’s proximity to Hong Kong.
The second patient (64F) is from Zhejiang Province and is a farmer who had contact with live poultry. She became ill on 30Oct13, was admitted to a local hospital on 31Oct13, and was transferred to another hospital on 03Nov13. She is currently in a critical condition.
An excellent article on CIDRAP News by Lisa Schnirring addresses two significant questions from these events with input from influenza experts: Is there another H7N9 wave coming and is there seasonality to H7N9? On both counts, it is still too early to tell. However, it is increasingly clear that the virus has not “burnt out” over the summer and disappeared. In addition, as pointed out by Recombinomics (here), the detection of a very mild case in a child through routine surveillance could suggest that the actual incidence rate in Guangdong Province may be much higher.
In addition, Recombinomics is tabling an additional concern. Sequencing data, obtained from earlier isolates, suggests two sub-clades of H7N9 are in human circulation, with one sub-clade in China’s NE and the other in southern China. The two sub-clades are distinguishable by differences in four internal gene segments (PB2, PB1, NP, NS). Does the new appearance of human cases in both the NE and southern China mean that both sub-clades have re-emerged this fall? (see Commentaries here and here.)
 WHO Confirms 23rd H5N1 Case This Year in Cambodia
WHO Confirms 23rd H5N1 Case This Year in Cambodia
06Nov13
The WHO has issued a press release yesterday announcing the 23rd case of human H5N1 infection in Cambodia this year. The patient (2F) “…from Svay Chrum village, Borng Bort Kandal commune, Bakane district, Pursat province was confirmed positive for H5N1 human avian influenza on 30th October 2013 by Institut Pasteur du Cambodge. The girl developed fever on 17th October 2013. On 19th October 2013, her parents sought treatment for her at a local private practitioner. Her condition worsened and she was admitted to Jayavarman VII Hospital in Siem Reap on 25th October 2013 with fever, running nose, lethargy, dyspnea, cough and breathing difficulties. Laboratory samples were taken the same day, but no Tamiflu was administered. The girl died on the 26th October 2013.”
These sad events push the fatality count in Cambodia for this year to 12 of 23 cases. They also advance the total number of H5N1 in Cambodia since the disease first entered the global stage roughly a decade ago to 44. While the latest victim was reported exposed to sick poultry two months ago, it is unclear whether that exposure is related to human infection. Governmental agencies in Cambodia are working to evaluate any epidemiological linkage among the 23 cases reported this year.
 22nd Case of Human H5N1 Infection Reported in Cambodia
22nd Case of Human H5N1 Infection Reported in Cambodia
31Oct13
The WHO and the Ministry of Health (MoH) of the Kingdom of Cambodia have reported, in a joint press release, the 22nd case of human infection by H5N1 influenza this year. The patient (6F) from Battambang Province is currently hospitalized in stable condition. The patient came down with a fever on 14Oct13, was hospitalized on 19Oct13, and tested positive for the H5N1 virus on 24Oct13.
It remains unclear why so many human H5N1 infections have occurred in Cambodia this year. After all, only 43 human H5N1 infections have been observed in Cambodia since its first case in 2005. To date, only half of the human cases this year have survived.
 Influenza: Quiet Rumblings in US
Influenza: Quiet Rumblings in US
31Oct13
The most recent data from the CDC (here) [for Week 42, ending Oct 19, 2013; the 3rd week of the 2013-2014 flu season] and the WHO (here) indicate that influenza activity in the Northern hemisphere, including the US, remains at inter-seasonal levels. the latest data, in graphical format, can be found here. Nationally, 3.8% of collected respiratory specimens tested positive for influenza. Most (83%) of the positive specimens were typed as influenza A (17% were influenza B). Most of the influenza A specimens were not further sub-typed, but the majority (>75%) of those that were sub-typed were found to be 2009 H1N1p. Similarly, 5.8% of all deaths reported through the 122-Cities Mortality Reporting System were due to pneumonia and influenza (P&I). This percentage was below the historic epidemic threshold of 6.2% for week 42. While forty-eight states and New York City experienced minimal ILI activity, two states did experience low ILI activity: TX and MS.
Beneath all of this data are a few tidbits the presage the coming season. for example, while the 3.8% of all respiratory samples tested were positive for influenza on a national basis, there was considerable regional variation (as per defined HHS surveillance regions). Thus, while certain regions also exhibited % positive specimens near the national average (e.g. the West with around 2% positive), other regions were well below (e.g. the Northeast near 0%). But notably, the SE weighed in at a whopping 12% of flu-positive specimens. Look for the ILI levels in the SE, which are still normal, to be among the first in the nation to elevate in the coming weeks.
 Gilead Reports HIV Suppression for Nearly 3 Years With Quad Tx
Gilead Reports HIV Suppression for Nearly 3 Years With Quad Tx
16Oct13
In a press release issued today, Gilead Sciences, Inc. is reporting the results of 2 pivotal Phase 3 studies on its single tablet, quad-inhibitor (elvitegravir 150 mg/cobicistat 150 mg/emtricitabine 200 mg/tenofovir disoproxil fumarate 300 mg), drug Stribild for HIV treatment. The two studies enrolled treatment-naïve patients with HIV-infection (> 5,000 copies/ml of HIV RNA) in a randomized, double-blinded trial construct. In one study, the comparator arm consisted of patients receiving the tripartite drug Atripla while in the other study patients received a protease inhibitor-based regimen of ritonavir-boosted atazanavir plus Truvada. Both studies found that, after 144 weeks of treatment, 78-80% of patients achieved HIV RNA (viral load) less than 50 copies/mL (based on the FDA snapshot algorithm).This compares to 75% of patients meeting this endpoint in either comparator arm.
The benefits to patients for Stribild are a convenient single, once-daily orally-administered tablet with slightly elevated efficacy and a more favorable safety profile: for one study, lower rates of neuropsychiatric side effects, lower treatment-induced increases in total cholesterol and LDLs and, in the other study, lower hyperbilirubinemia and a lower change from baseline in spine bone mineral density. It should be noted that “Stribild has a Boxed Warning on the risks of lactic acidosis/severe hepatomegaly with steatosis and post treatment acute exacerbation of hepatitis B…” Nonetheless, these studies further progress the therapeutic opportunities available to HIV patients in their unending battle against the virus.
 New Influenza Season Starts in US & Canada
New Influenza Season Starts in US & Canada
16Oct13
From a purely record keeping standpoint, the 2013-2014 influenza season has started in the northern hemisphere, including the US. Due to the government shutdown, it is impossible to get an early read on current influenza activity in US. However, the WHO has issued a global flu update and virological update on Oct. 14th that helps shed some light. As perhaps expected for the “inter-seasonal period”, “In general, influenza activity was low in the northern hemisphere and moderate-to-sporadic in the southern hemisphere.” Flu activity is starting to increase in Europe, though still low, while flu was moderate-to-sporadic in the southern hemisphere. For the two weeks ending 29Sept13, WHO GISRS laboratories tested more than 17,704 specimens. Of these, 1277 (7.2%, a somewhat high percentage for this time of year)) were positive for influenza viruses, of which 996 (78%) were typed as influenza A and 281 (22%) as influenza B.
Data from the US is harder to come by. Online flu-tracking sites are generally reporting an increase in flu activity [still in the low-moderate range], though these reports are largely based on aggregating anecdotal reports. These same tracking organizations show increased flu activity in western Canada. In an unusual occurrence this early in the season, an adult flu-related fatality has been reported in Dallas County, TX.
 China Reports H7N9 Vaccine Ready for Human Use
China Reports H7N9 Vaccine Ready for Human Use
31Oct13
China’s official news agency, Xinhua, is reporting that Chinese scientists from five institutions have collaborated to produce a vaccine against the H7N9 avian influenza virus. The vaccine candidate has progressed through testing in ferrets (the gold standard model for influenza) but additional testing is required before deployment in humans.
The path to the vaccine began with a throat swab from a human H7N9 patient last Spring and involved the use of reverse genetics to create the final vaccine candidate. "Our new vaccine has been tested by various institutions, including Zhejiang University, as well as Hong Kong University - and it meets international standards. In the past, we used to import vaccines, but now, we make them ourselves." As experts express renewed worries about an upcoming winter epidemic of H7N9 (see here), successful testing must be completed soon to allow for distribution and uptake in at-risk populations.
On a related matter, another team of scientists from China is reporting in The Lancet that promptly shutting down some 780 live poultry markets [LPMs] in major cities last Spring had a dramatic impact on the spread of H7N9. "Closure of LPMs reduced the mean daily number of infections by 99% (95% credibility interval 93—100%) in Shanghai, by 99% (92—100%) in Hangzhou, by 97% (68—100%) in Huzhou, and by 97% (81—100%) in Nanjing. Because LPMs were the predominant source of exposure to avian influenza A H7N9 virus for confirmed cases in these cities, we estimated that the mean incubation period was 3·3 days (1·4—5·7)." The authors conclude that closing LPMs is a viable and highly effective intervention strategy where markets overlap known infection of people or poultry.
But closing LPMs is an expensive proposition for the Chinese economy. Last May, an article in Reuters reported that the Spring H7N9 outbreak had cost the Chinese economy roughly $6.5B. Thus, it is likely that future, possibly prolonged or more numerous closures would be met with stiff resistance at some point.
If there is a winter outbreak of H7N9 on the horizon, one can be sure that both of these tools will be employed to mitigate the severity of the outbreak.
 China Reports 2nd Human H7N9 Case of 2013-14 Flu Season
China Reports 2nd Human H7N9 Case of 2013-14 Flu Season
23Oct13
China’s official news agency, Xinhua, is reporting a second case of human H7N9 infection this fall. The new case (67M), a farmer near Jiaxing in Zhejiang Province, was admitted to the hospital on Oct. 16th and is currently in serious condition. The first confirmed case of human infection by H7N9 this fall was reported just last week (see below).
In the spring and early summer of the 2012-2013 flu season, the H7N9 virus made its initial appearance as a human pathogen, infecting some 135 individuals in China and Taiwan, leaving 45 dead.
Recombinomics, in two recent Commentaries (here and here), has noted sequence differences between two isolates from the first new case this fall (collected, sequenced, and released by the Zhejiang University and Zhejiang CDC) and the consensus H7N9 sequences from human isolates collected around Shanghai and adjacent provinces earlier this year. Over all, the sequences from all 8 gene segments matched quite well between the two sets. However, Recombinomics notes that the PB2 sequences differ, with one of the Fall 2013 isolates missing mammalian adaptation markers (such as E627K) while the other isolate "...had D60N and D87N. The latter is a mammalian adaption which produces an increased polymerase activity at lower temperatures (33 C), consistent with a higher viral load in a human nose in the winter. This temperature sensitive activity is also found in PB2 with E627K." The H7 HA genes from the Fall isolate are quite similar to the consensus sequence and contains Q226L but also Q222P.
These first glimpses into the H7N9 virus as it returns from its summer holiday are particularly relevant to the ongoing controversy over "gain-of-function" experiments that seek to define the genetic and molecular basis for human pathogenicity of influenza viruses. An article today in Reuters by Kate Kelland nicely summarizes the controversy. If the genetic and molecular signatures that convey high pathogenicity for a given influenza virus in humans can be defined, then the naturally occurring changes in the virus can be assessed more quickly and confidently. However, such molecular and genetic detective work is not without its critics, who worry about safety issues (accidental release of a highly virulent flu strain) and the value of the experimental results. Regardless of the debate among experts, the H7N9 virus will continue to change and adapt, seeking new advantage as the influenza season commences in China.
 Human H5N1 Cases Reach 21 in Cambodia This Year
Human H5N1 Cases Reach 21 in Cambodia This Year
23Oct13
The WHO and the Ministry of Health (MoH) of the Kingdom of Cambodia have reported today another confirmed case of human H5N1 infection, the 21st this year. The patient, an 8-year-old girl from O-Raing village in Kampong Thom province was confirmed positive for H5N1 influenza on 17th Oct by Institut Pasteur du Cambodge, and was admitted to the hospital, on 11th Oct, with fever, cough, vomiting and dyspnea. Tamiflu administered on 14th Oct and the patient is currently in a stable condition. The girl is believed to have come in contact with infected poultry when she help prepare a meal using a chicken that had already died from H5N1.
Only 10 of the 21 individuals infected in Cambodia this year have survived. Since 2005, Cambodia has had an aggregate of 41 cases of human infection by H5N1. The reasons behind the high number of cases this year in Cambodia remain unclear.
 China Reports 1st H7N9 Case of 2013-14 Flu Season
China Reports 1st H7N9 Case of 2013-14 Flu Season
15Oct13
China’s official news agency, Xinhua, is reporting a new case of human H7N9 infection, the first of the 2013-2014 influenza season in the northern hemisphere. In the spring and early summer of the 2012-2013 flu season, the H7N9 virus made its initial appearance as a human pathogen, infecting some 135 individuals in China and Taiwan, leaving 45 dead.
The new case (35M), a resident of Shaoxing County in Zhejiang Province, was admitted to the hospital on Oct. 8th and is currently in critical condition.
Hope has been expressed that the H7N9 influenza would not make a return appearance in the fall. These hopes were largely pinned on the massive culling of poultry and live market closings that occurred in China last spring. Limited duration appearances of human influenzas are not without precedence (e.g. the H2N2 pandemic of 1957/58 that disappeared from human circulation by 1968). With the influenza surveillance protocols currently in place in China, the next few weeks will tell the tale about a possible reappearance of human H7N9 infections.
 Global MERS-CoV Count Climbs to 136
Global MERS-CoV Count Climbs to 136
11Oct13
Last week, the WHO issued a GAR (on Oct. 4th, here) confirming 6 news cases of human MERS-CoV coronavirus infection to the global count. All 6 cases (3M/3F, all from the region around Riyadh) were from the Kingdom of Saudi Arabia (KSA). This brings the global total of human infection by MERS-CoV to 136 with 58 deaths. Of that total, fully 117 of these cases originated in the KSA, including 49 of the 58 deaths.
All eyes are now on the impending Hajj pilgrimage to the KSA where roughly two million Muslims from across the globe will congregate. No travel restrictions have been put in place, but many are worried about the opportunity for global spread of the virus (see for example, here and here). The main worry in this regard is the incubation time for infected individuals (on the order of 5 days). Infected, asymptomatic individuals could return from the Hajj, thus requiring some degree of post-travel monitoring. Especially in the poorest countries and the US, this is now unlikely to occur.
 Shutdown Halts Disease Surveillance
Shutdown Halts Disease Surveillance
11Oct13
The Republican Party-enforced government shutdown has created extensive hardship across the country. Among the difficulties created by this action is a suspension of important public health activities, including the monitoring of food safety and infectious disease outbreaks. Two current infectious disease threats to the public are lacking adequate surveillance because government agencies are shut.
Readers familiar with these pages are well aware that the global threat from influenza is, right now, a matter of some concern, especially in Asia. With several influenza strains circulating that have proven pathogenicity in humans (e.g. H5N1, 2009 H1N1p, and H7N9), the region is a bubbling cauldron of potential genetic "remakes" that could produce a deadly virus that readily transmits to/among humans. As noted by Michael Smith writing for MedPage Today (here), the flu season has commenced in the US and is “unfolding largely unobserved”. Specifically, “…That means information about such things as pediatric influenza, anti-viral resistance, admissions to hospital for flu or flu-like illness, and mortality and morbidity owing to pneumonia and influenza is not being gathered.”
In reality, the problem is larger than just the flu. The MedPage Today article, in quoting Dr. Gregory Poland at the Mayo Clinic, states that "There are an endless number of infectious disease threats that, as we often say, are an airplane ride away from us," Poland said. And the CDC is the "only entity" that tracks infectious disease on a national scale, he added. "So now you've got a week, 2 weeks, who knows how long, where there's no one really responsible for watching what's happening nationally." For example, the Hajj is about to commence starting on Oct. 13, with millions of pilgrims traveling to Mecca, to a country that is in the midst of the MERS coronavirus outbreak. Thus, the real worry is that, with no one watching, a US-based outbreak could establish much more of a foothold in country before the threat is recognized.
A surrogate indicator for the potential risk to the nation’s public health was delineated earlier in the week when a food-borne outbreak of antibiotic-resistant salmonella sickened some 300 in 20 states and Puerto Rico (see here, here, and here), with nearly half (42%) of the victims hospitalized. The culprit was quickly identified as raw chicken packaged by Foster Farms in California. Although the CDC quickly recalled 30 furloughed staff to deal with the outbreak, it is hard to judge the extent (and even control) of such outbreaks if oversight agencies are understaffed. As noted today by Dr. Richard Besser, ABC News’ chief health and medical editor, “I have to tell you that the outbreak is still going on. There were three new cases yesterday. Until this is over, I would still stay away from this chicken.” The latter comment was made, in part, because of the unusual number of hospitalizations that have resulted in this outbreak.
When the very instruments of government are hijacked as tools to further the interests of a political party, society as a whole suffers. When it comes to infectious diseases, the sentinel duties performed by government are crucial, especially in an age of rapid global transit, and impeding the ability of government to perform such essential duties puts all citizens are greater risk of significant illness and even death.
 Another HIV Vaccine Trial Disappoints
Another HIV Vaccine Trial Disappoints
10Oct13
In a new article just published in the New England Journal of Medicine, the HIV Vaccine Trials Network 505 Study team has published the results of a Phase 2b efficacy trial of the latest HIV vaccine construct: a DNA prime–recombinant adenovirus type 5 boost (DNA/rAd5) vaccine regimen in persons at increased risk for HIV-1 infection. As noted in the article, “The 6-plasmid DNA vaccine (expressing clade B Gag, Pol, and Nef and Env proteins from clades A, B, and C) was administered at weeks 0, 4, and 8. The rAd5 vector boost (expressing clade B Gag-Pol fusion protein and Env glycoproteins from clades A, B, and C) was administered at week 24.” A test group of 2504 subjects (men or transgendered women who have sex with men) received either the DNA/rAd5 vaccine or placebo. The trial “…assessed HIV-1 acquisition from week 28 through month 24 (termed week 28+ infection), viral-load set point (mean plasma HIV-1 RNA level 10 to 20 weeks after diagnosis), and safety.”
Unfortunately, the DNA/rAd5 vaccine neither reduced the rate of HIV-1 infection nor met the secondary viral set point (viral load after infection but prior to anti-retroviral therapy) target specified in the protocol. As a result, the “…data and safety monitoring board recommended halting vaccinations for lack of efficacy..” earlier this year. The vaccine did, however, elicit both cellular and humoral immune responses.
The trial embodies the dilemma faced today in the HIV vaccine space. With over 2 million new infections each year globally, new infections still out-pace the number of patients initiating anti-retroviral therapy. However, critics believe that this particular trial was unwise to execute. In an article in MedPage Today, Carlos del Rio, MD, of Emory University was relieved that the trial was not harmful to any patients. Dr. Rio was an investigator in an earlier study (the STEP trial) that also employed a recombinant adenovirus-5 vector. In the STEP trial, this vector “…appeared to be associated with the increased risk of HIV among those who got the vaccine candidate.” Quoting Dr. Del Rio, the article states that "The study should never have gone forward," he said. "The scientific rationale to do it, after STEP, was in my mind not there." Quoting further, “”There's such an urgency to find an effective vaccine," Del Rio said, that investigators might have jumped the gun.”" The investigators in the present study disagree, however, noting that the adenovirus-5 vectors are not the same in the two studies; the present study’s vector contains less of the adenovirus genome and includes the HIV env gene.
Biomedical investigators learn more about HIV and its interaction with the human immune system with every trial. Efforts aimed at identifying broadly neutralizing, potent anti-HIV antibodies in long-term non-responders does demonstrate that, at least in some small fraction of the human population, a beneficial immune response can be mounted. But the central question remains: How do we educate a “typical” human immune system to respond with efficacy to such a cagey viral intruder?
 Human H5N1 Cases Reach 20 in Cambodia This Year
Human H5N1 Cases Reach 20 in Cambodia This Year
19Sept13
A news report out of China relates confirmation that an additional two cases of human H5N1 infection have occurred in Cambodia. The two patients (5F and 2F) come from two different, adjoined provinces, Takeo and Kampot, respectively. Sadly, the 2F patient passed away on Wednesday. The 5F patient is reportedly hospitalized in stable condition.
This year’s total cases of human H5N1 infection in Cambodia now stands at 20, nearly half of the total of 41 cases reported from Cambodia since 2004. Eleven of the aggregate 30 fatalities since 2004 have occurred this year, yielding an approximate case fatality rate of 55%. As of August, 2013, the WHO has reported 27 cases of human H5N1 infection globally this year, with 18 associated fatalities (Cambodia is listed in this report with 17 YTD cases and 10 fatalities).
 MERS-CoV: Extensive Recombination & More Cases of Human Infection
MERS-CoV: Extensive Recombination & More Cases of Human Infection
20Sept13
A number of Commentaries from Recombinomics over the past few days (here, here, and here) analyzed a set of 45 MERS-CoV sequences, spanning cases from 2012-2013, that were just released by the Kingdom of Saudi Arabia’s Ministry of Health. Included within this set is a group of complete viral sequences from 13 cases. Within the scope of the 3 cited Commentaries, three distinct examples of viral recombination are illuminated. These examples are important because evidence of viral recombination suggests that the incidence of MERS-CoV infections in humans is much, much higher than suggested by the number of confirmed cases. Moreover, these observations suggest rapid viral evolution/adaptation in the human population, a suggestion with potentially ominous overtones.
In example 1, two isolates (EMC/12 and Bisha_1_2012) from the same patient, taken six days apart in 2012 (EMC/12 on June 13th and Bisha_1 on June 19th), are nonetheless dramatically different. EMC/12 was the first sequence ever made public. Along with another early sequence (Jordan-N3), EMC/12 constitutes a distinct sub-clade (from the England1/2012 sub-clade) with shared polymorphisms clustered around a particular gene locus (characteristic of recombination events). In contrast, the Bisha_1_2012 sequence is more closely related to more recent sequences and showed evidence of additional recombination within this subclade by distinct clustering of shared polymorphisms. Thus, this early patient was likely infected by at least two very distinct MERS coronaviruses.
In example 2, a full sequence obtained in Oct. of 2012 (Riyadh_1_2012) is observed to be virtually identical to Bisha_1. Thus, Recombinomics notes that “…the identities between the two sequences from samples collected 4 months apart at well separated locations, also seriously limits the use of a molecular clock for the determination of a near term jump of MERS to humans.” In addition, new results just published in The Lancet by Cotton et al. (paper here) show three distinct MERS-CoV genotypes identified in Riyadh alone.
In example #3, the Hafr-Al-Batin_1_2013 sequence shows even more extensive signs of recombination. “The sequence had clear clustering of polymorphisms from four different parents. Positions 542-1833 had 5 polymorphisms shared with Jordan-N3. The sequence between positions 3276-19418 then switch to an Al Hasa sequence with 8 polymorphisms shared with Al Hasa 1-4. The sequence then changed again with 3 UAE polymorphisms between 20848 and 22895. The sequence then switched back to Al Hasa with 6 polymorphisms between 23648 and 24740. The 3’ end of the genome had 6 England1 polymorphisms between positions 25052 and 29853.”
Thus, our picture of MERS-CoV has changed significantly. These data no longer support the notion of a recent jump to humans via a single zoonotic event and subsequent rapid viral evolution. Indeed, data presented in The Lancet paper suggest that the virus was circulating in humans for at least a year prior to its documented emergence and the actual emergence could have occurred as early as 2007. Further, the dynamics of zoonotic transmission appear to be intermittent and complex; the zoonotic source(s) of MERS-CoV remains elusive. As summarized in the paper of Cotton et al., “Multiple introductions of MERS-CoV are identified and suggest lower R0 values. Transmission within Saudi Arabia is consistent with either movement of an animal reservoir, animal products, or movement of infected people. Further definition of the exposures responsible for the sporadic introductions of MERS-CoV into human populations is urgently needed.”
These new finding come against a backdrop of additional new cases identified in the Kingdom of Saudi Arabia [KSA]. According to the latest Global Alert & Response from the WHO (dated 20Sept13; here), a total of 130 laboratory-confirmed cases of infection with MERS-CoV have been documented globally, with 58 deaths. This tally reflects a change in the designation from “confirmed” to “probable” of two earlier cases out of Italy. This GAR comes, in turn, on the heels of the WHO confirming an additional 18 cases, all out of KSA, earlier in the week (see here). This represents an increase of 30 cases since the end of August: a roughly 30% increase in just three weeks.
 Progress on MERS-CoV As Cases Jump to 130
Progress on MERS-CoV As Cases Jump to 130
10Sept13 Updated 12Sept13
Just as eight new cases of MERS-CoV cases were reported over the past few days by the Kingdom of Saudi Arabia’s [KSA] Ministry of Health [MoH] (see here and here), new hope is emerging for therapeutic and prophylactic intervention. The most recent announcements of cases come on the heels of confirmation by the WHO of 4 other MERS-CoV cases reported last week by KSA’s MoH (see here). Three fatalities are included among the most recent reports and the unofficial global case count now stands at 122 with 57 fatalities. Fully 98 of these cases are reported from the KSA. As noted in an article by CIDRAP News (here), it is of continuing concern that “Of the 12 case-patients, at least 7 had contact with a confirmed MERS patient or worked in a hospital with another confirmed case-patient.” A new report out on 12Sept13 from CIDRAP News adds another 8 cases in KSA, pushing the global number of cases of human infection to 130.
As further noted in the former CIDRAP article, “Reaction from experts to news of the cases ranged from reassuring to concerned.” Much of the concern is centered on the ongoing rate of new cases that, despite much new information about the virus and an ever-increasing time line, persists at a fairly constant rate. It is a bit like poker. At any given point in time, in the modern globalized world, there is a finite risk that the virus could travel to a part of the world where health care resources and infection control are lower or absent, touching off a substantial increase in human cases of infection and allowing even greater geographical spread. The longer the game keeps going (the longer these infections go on) the greater the chance that someone in the game will draw a straight flush. To combat this such, many are calling for better communication and sharing of data to “end the game as early as possible”.
In the meantime, a new paper, appearing in Nature Medicine as an advance online publication, describes the ability of interferon-alpha2b together with ribavirin to reduce signs of pneumonia (no development of breathing abnormalities or radiologic evidence of pneumonia) and reduce pro-inflammatory markers in virally-challenged rhesus macaques as compared to untreated but similarly infected animals. Treated animals also showed less severe histological changes in the lung and lower viral loads. Though relatively expensive, this drug combination has a proven clinical track record in the treatment of hepatitis C patients and would be a welcome addition to the clinical quiver after additional successful testing, possibly even as an early intervention therapy.
And finally, there was positive news for MERS-CoV propylaxis at the end of last week as a European academic coalition announced the successful creation of a MERS-CoV vaccine (see here). The candidate vaccine is constructed from a modified Vaccinia Ankara [MVA] framework and bears the MERS-CoV spike (S) protein. The coalition has shown that the MVA-MERS-S vaccine candidate can induce anti-MERS-CoV antibodies against the spike protein in mice. These induced antibodies can also block MERS-CoV infection in vitro. The team’s work is described in the latest edition of the Journal of Virology (see here) On a related note, a team from Spain has just reported another potential vaccine candidate involving a recombinant MERS-CoV construct absent the structural E protein that is replication competent but able to propagate (see the Paper).
Further testing and development of these candidate vaccines could lead to safe and efficacious product that would certainly be a key emergency tool in the control and containment of a deadly emergent disease. However, the testing and development of a MERS-CoV vaccine is still years away from any widespread use in humans (see here).
 Homing In on H7N9 Human Tropism
Homing In on H7N9 Human Tropism
10Sept13
Two new scientific studies mark further advancement in our understanding of how H7N9 is able to infect human airways, often to devastating consequence. One of the studies appeared online at the American Journal of Pathology (see here) from Thijs Kuiken’s group at Erasmus University Medical Centre. This report describes histo-chemical findings on the binding of viruses, genetically engineered to contain the hemagglutinin (HA) from either of two strains H7N9 (A/Shanghai/1/2013 or A/Anhui/1/2013), to formalin-fixed human respiratory tract tissues.
The team found that the engineered viruses “attached moderately or abundantly” to both upper and lower respiratory tract specimens. The team has not observed such as pattern of binding previously with any other influenza A virus. The implication of these observations is that the H7N9 virus can efficiently bind to the upper airway epithelium, enabling ready human-to-human transmission via aerosol or droplets, and can bind to the lower lung epithelium causing pneumonia and severe disease.
The second study Is a remarkable paper from George Gao and a multi-institutional team in China, giving the detailed molecular structure of the viral HAs from the same two H7N9 strains, both by themselves and in complex with avian and/or human receptors. The work is now online at Science in advance of publication (here). In this report, the A/Shanghai/1/13 strain’s HA was found to bind preferentially to analogs of avian receptors while A/Anhui/1/2013 binds to analogs of both human and avian receptors. One molecular difference between the two HAs is the presence of Q226L in A/Anhui/1/2013 (and most other H7N9 human isolates). As noted in the report, “Recent work has shown that the Q226L (H3 numbering used throughout) substitution in avian H5N1 HA confers human receptor (α-2,6-linked to galactose) binding and simultaneously significantly reduces avian receptor (α-2,3-linked galactose) binding.” To test whether this amino acid difference at position 226 solely accounts for the shift to binding of human receptor binding, a L226Q mutant form of A/Anhui/1/2013 HA was generated. The L226Q mutant H7N9 virus retained its parental dual receptor specificity (although with roughly 10-fold weaker binding to a human receptor analog) suggesting that molecular attributes other than L226 are responsible for the dual receptor specificity in the HA of A/Anhui/1/2013. The two viral strains also differ from each other at three sites in the receptor binding site: S138A, G186V, and T221P.
All of this matters since the mechanisms by which flu viruses evolve to efficient transmission in humans are of critical epidemiological concern. The fact that H7 viruses including the initial human isolate A/Shanghai/1/13, possess weak, though discernable, binding to human receptor analogs while the A/Anhui/1/2013 strain exhibits marked binding to these same human receptor analogs (though this alone is insufficient for ready human-to-human transmission) illustrates the complexity of these mechanisms.

West Nile Virus Outbreak -Update
29Aug13
The most release of data from the CDC shows the number of cases of WNV nationwide continues to climb. The current number of confirmed cases of WNV is 421, of which 197 are the more worrisome "neuroinvasive" sub-type, including 13 deaths. This compares to 296 total cases as of last week. Eight additional states reported cases last week for the first time this season for a total of 35 states reporting. For example, Massachusetts just reported its first case of WNV this year. Last year, the state had 33 cases with one fatality. The incidence of WNV this year continues to be a fraction of last year's pace where, for the week ending Aug. 28th, 2012, some 1590 cases were already tallied.
Select DAAs in Development for Oral IFN-Free Regimens for HCV
Drug
Inhibitory Target
Owner
Simeprevir
Protease
J&J/Medivir
Sofosbuvir
Polymerase (NS5B)
Gilead
Daclatasvir
NS5A
BMS
 H7N9 Influenza: Another Fatality & More
H7N9 Influenza: Another Fatality & More
21Aug13
The human H7N9 influenza death toll increased once more with the passing of two more patients (see here and here). One patient (case #134; 61M from Hebei Province, hospitalized on July 18th) passed away on the 11th of August from multiple organ failure and was the 44th H7N9 fatality this year. No details were provided by Chinese authorities on fatality #45 as of this writing.
In the meantime, scientists are eagerly anticipating the next set of experimental data on an H7N9 vaccine. In a great piece by Helen Branswell of the Canadian Press, it is noted that "Four flu vaccine manufacturers have started or will soon start clinical trials on H7N9 vaccines, with four more expected to conduct trials in the late fall or early winter..." Quoting Dr. Robin Robinson, director of the Biomedical Advanced Research and Development Authority, the article further notes that """We're just trying to get some indication that the vaccines are immunogenic and certainly well tolerated and that the adjuvants are providing some antigen-sparing effect," Robinson says, adding that preliminary results could be available in October or November." You may recall that early reports expressed some concerns about the immunogenicity of H7N9 in humans, suggesting that efficacious vaccines may be hard to come by for H7N9. since then, several companies have reported successful generation of immune responsiveness in preclinical studies, so we shall soon see.
The importance of having an efficacious vaccine for H7N9 was underscored once again with a new report appearing in the Sept., 2013 edition of The Lancet by Dr. Yuen Kwok-Yung and colleagues at the University of Hong Kong. As noted by news stories covering the publication of this work (such as here), these investigators tell the tale of two influenza viruses (H5N1 and H7N9) impacting two major cities (Hong Kong by H5N1 in 1997 and Shanghai by H7N9 in 2013) that share many common characteristics. But importantly, Dr. Yuen notes that H7N9 apparently jumps from birds to humans at unprecedented speeds, faster than all known strains of the bird flu virus, including H5N1. Why this is the case is not yet clear, but may be related to the low pathogenicity of the virus in birds. In contrast, H5N1 clearly announces its presence in the avian community by killing many infected birds. Regardless, the control of a new H7N9 outbreak this fall, should it occur, is more challenging without avian sentinels.
In an interesting development, Dr. Yuen has noted the possible spread of the H7N9 virus via human fecal transmission. In a systematic evaluation of tissue-specific viral loads and corresponding histopathology, it was concluded that fatal H7N9 cases were “…characterized by viral and secondary bacterial pneumonia with 67% having positive RT-PCR in stool.” In an interview with the South China Morning Post, Dr. Yuen stated that “This has important implications on the infection control strategies for H7N9 virus infection, as the influenza virus in stools may contaminate the surrounding environment…". The article goes on to note that
“…the team also suggested that the fact the virus may be transmitted via faeces was the reason why, so far, few cases of human-to-human infection had been recorded, Yuen said.” Dr. Yuen notes that, aside from the presence of the H7N9 virus in stool samples, there is as yet no evidence to support the notion of viral transmission via human contamination of the environment. Nonetheless, it is an intriguing idea worthy of further investigation.
 Arboviruses on Stage in U.S.
Arboviruses on Stage in U.S.
21Aug13
It is summer and with the season comes the return of a set of mosquito-borne diseases to the U.S., including dengue (DEN), West Nile virus (WNV), and Eastern equine encephalitis (EEE) virus.
Yesterday, the Massachusetts Department of Public Health announced the first EEE fatality for 2013. The patient (85F) was hospitalized in mid-August and died several days later. Nationally, only 3 other confirmed EEE cases have been reported so far this year: 2 in Florida and 1 in Georgia. According to the CDC, EEE "...is one of the most severe mosquito-transmitted diseases in the United States with approximately 33% mortality and significant brain damage in most survivors." Most people infected with the virus remain asymptomatic but the disease can progress "...to a more severe form with symptoms such as the sudden onset of headache, high fever, chills, and vomiting. The illness may then progress into disorientation, seizures, or coma."
Last week, three local cases of DEN were reported in central Florida. According to the press report, "The Florida Department of Health says the three patients are residents of Martin and St. Lucie counties. Officials say the patients acquired dengue from mosquitoes in Rio, near Jensen Beach. None have traveled internationally recently. Officials say St. Lucie County hasn't had any cases of locally acquired dengue until now. There was one case in Martin County in 2011." As noted in a recent News Watch story from National Geographic, "Reports of dengue fever were rare in Florida until 2009 when physicians began diagnosing cases around Key West in individuals who had not traveled outside the state." Earlier this year, NPR recounted that "Dengue fever was endemic in the U.S. before World War II, until the U.S. Army led aggressive mosquito-eradication campaigns to among troops. Their efforts wiped out malaria in the U.S. and took dengue along with it. But in the past decade or so, the virus and its primary transmitter, the Aedes aegypti mosquito, have been slowly back into Florida." Puerto Rico has been laboring under much higher levels of local dengue infections for some time, with over 4100 local dengue cases reported by the CDC already this year.
Finally, WNV cases are expanding rapidly on the U.S., with the case count roughly doubling each of the past three weeks. The latest data from the CDC tallies 301 cases to date, occurring mainly in a swatch running from Minnesota to southern California. Minnesota and the Dakotas account for over one third of all cases so far this year. Roughly half of all reported cases are of the more deadly neuroinvasive type and 11 deaths have been reported this year to date. California has alone has reported 4 deaths and 20% of all cases. Last week's case count (as of August 13th) stood at 174 with 7 fatalities. Last year's WNV tally was one of the highest since the virus first arrived in the U.S. in 1999 with a total of 5,674 cases of human infection, including 286 deaths. WNV is very difficult to predict in terms of morbidity, mortality, and geographic location but 2013 levels appear far below those observed last year: By Aug 28th of 2012, a total of 1590 WNV cases were reported nationwide.
 Antibodies to MERS-Like Virus Found: The Animal Source for Human Infection by MERS-CoV?
Antibodies to MERS-Like Virus Found: The Animal Source for Human Infection by MERS-CoV?
09Aug13
The hunt for the animal source of infection for the MERS-CoV virus currently active in the Middle East, has been the subject of intense research efforts. In a paper appearing today in The Lancet, an international team of scientists has now performed a comparative serological survey of assorted livestock species [Cattle (n=80), sheep (n=40), goats (n=40), dromedary camels (n=155), and various other camelid species (n=34)] from Oman, the Netherlands, Spain, and Chile. They analyzed blood samples for the presence of antibodies specific to MERS-CoV, to the SARS coronavirus, and to the human coronavirus HCoV-OC43. They found that “50 of 50 (100%) sera from Omani camels and 15 of 105 (14%) from Spanish camels had protein-specific antibodies against MERS-CoV spike. Sera from European sheep, goats, cattle, and other camelids had no such antibodies. MERS-CoV neutralising antibody titres varied between 1/320 and 1/2560 for the Omani camel sera and between 1/20 and 1/320 for the Spanish camel sera. There was no evidence for cross-neutralisation by bovine coronavirus antibodies.” Clearly, MERS-CoV or a immunologically-related virus has infected camels, extensively so in Oman.
These observations raise the possibility that camel may be an important animal reservoir for MERS-CoV, though additional studies are in order to define what role camels play in the transmission of virus to humans. Previously, bats have been suggested as a potential reservoir. But, as clearly delineated (for example, see here) by Recombinomics, the sequences of MERS-CoV and bat beta2c coronaviruses are in fact quite far apart. In fact, no MERS-CoV-like viral polymerase sequence has been identified in bats. Hopefully, the present study constitutes an important step towards eventual identification of the zoonotic source of MERS-CoV.
As of yesterday, the number of confirmed cases of MERS-CoV infection in humans now stands at 94 with 46 deaths. For a summary of the case count by country, the reader is referred to this CDC webpage.
 Honduras Declares State of Emergency Due to Dengue
Honduras Declares State of Emergency Due to Dengue
01Aug13 Updated 05Aug13
The government of Honduras has declared a state of emergency due to a dengue fever outbreak that has killed 16 people and sickened 12,000, according to news reports out yesterday. In response, the government is making it a priority to control the disease by fighting the mosquitoes that spread it. Already, more than half of Honduras' municipalities have registered dengue fever cases.
Overall, there appears to be many locales reporting much higher case loads of dengue this year. In February, Brazil reported over 200,000 cases in just the first 2 months of 2013, triple last year's case incidence. Roughly half of the cases were caused by the DENV-4 strain of the virus, which was first detected in Brazil in 2011. By July 31, Honduras, Costa Rica, Nicaragua and El Salvador have issued formal alerts. In Guatemala and Panama, officials say they are monitoring the disease, which normally spreads more easily later in the rainy season. The WHO has already noted that, by early July, dengue cases were up some 76% in Central America.
These developments are most striking in the context of recent historical data from the region. The table entitled "Dengue Morbidity and Mortality in the Americas: Honduras, Brazil, and Puerto Rico" (found here), shows the marked growth in dengue incidence over the past decade in the three listed countries. This is clearly a disease spiraling out of control, especially since programs to limit Aedes aegypti, the mosquito vector for the dengue virus, were wound down in the 1970's.
Of particular interest is the observation that Honduras has exhibited a severe disease index ([# of cases of severe dengue / # of total dengue cases] *100) above 10 for each of the past three years and 5 out of the last seven years. Typically, this index is somewhere around 1-3% (see graph, here), though certainly other countries have on occasion exhibited indices above 10. Nevertheless, the scope of new dengue cases in the Americas is in line with the rising global pattern of dengue that places 1/3 of the world's population at risk each year.
There are currently no therapeutics for dengue though a handful of vaccine candidates are under active development. The most advanced of these is a vaccine candidate from Sanofi SA, but clinical trial shortfalls and recent research insights that suggest new directions are needed for in vaccine design [for example, see here and here] may suggest that a safe and effective vaccine is still years away. Compelling action is needed now to mitigate a growing public health crisis.
 Cyclosporiasis Update
Cyclosporiasis Update
09Aug13
The CDC has updated the case count for the cyclosporiasis outbreak in the U.S. For the latest data, please go see this webpage. As of August 8th, a total number of reported cases has risen to 514 distributed among 17 states and NYC. This is up from 400 reported cases on August 1st. Most of the increase (77/114 cases) have been reported in Texas.
Nebraska and Iowa have conducted an investigation as to the source of the cyclosporiasis outbreak and have reported to the CDC that infections in their states are due to contaminated salad mixes (see the CDC webpage). It is not yet clear if the cases observed in other states is due to the same source.
 Outbreak of Influenza at Arkansas Cancer Center
Outbreak of Influenza at Arkansas Cancer Center
07Aug13
The CDC and the Arkansas State Health Department are investigating the unusual outbreak of a cluster of H3N2 influenza cases at a cancer treatment center at the University of Arkansas for Medical Sciences, according to a news report. Of the 31 reported cases, 29 cancer patients and one family member have tested positive for influenza A/H3N2. H3N2 was the dominant strain circulating in the U.S. this past flu season. The treatment center specializes in the multiple myeloma, so most of the patients are immunocompromised. All of the cases have apparently developed in the past week or so. At-risk individuals are currently being treated with Tamiflu. A cluster of influenza cases this time of year is unusual, though not unprecedented.
 Another Swine H3N2v Infection in Humans - ex Illinois
Another Swine H3N2v Infection in Humans - ex Illinois
02Aug13
The Illinois Department of Public Health (IDPH) laboratory has confirmed the 15th case of human infection by variant swine influenza virus, H3N2v. According to the IDPH press release, "The confirmed case is a Boone County child with mild symptoms who had contact with swine while helping an exhibitor at the DuPage County Fair which was held in late July." Illinois joins Indiana (with 13 confirmed cases) and Ohio (with 1 confirmed case) in reporting cases this summer. this is the first confirmed case of H3N2v infection this year; Illinois had a total of 4 human H3N2v cases last year.
As noted by Recombinomics, genomic sequencing of the recent Ohio case (who developed the flu after attending an agricultural fair in NW Virginia) showed that the viral HA was bearing the N145R mutation. N145R was also found in the H3N2v sequences emanating from Hancock county fair in Indiana. N145R has not been observed previously in swine isolates, suggesting it is a marker of human adaptation. Recombinomics further notes that "The earlier sequences in Indiana (from attendees of the Grant County Fair) had N145K, which also had not been previously reported in human cases, although this polymorphisms did appear in early 2013 swine H3N2v sequences." In addition, "The latest sequence from the Ohio DoH sample also has a novel constellation of genes, which includes H1N1pdm09 PA, which also has never been reported in humans (or swine). Five of the gene segments (PB2, H3, NP, N2, MP) are closely related to the 2013 Indiana H3N2v cases. However, the other three gene segments (PB1, PA, NS) have been circulating in recent H3N2v swine (which have internal genes closely related to human sequences from 2011) and two of the genes (PB1 and NS), are closely related to the sequences from 2012 Minnesota H1N2 cases." Sequencing data from the most recent Illinois case should prove to be quite illuminating.
 Two More Swine H3N2v Infections in Humans
Two More Swine H3N2v Infections in Humans
26Jul13
Two more confirmed cases of H3N2v infection have been reported by the CDC, bringing the case count to 14 for H3N2v infections this year. The two cases occurred in Indiana and Ohio. As noted by Recombinomics, exposure in the Ohio case actually occurred in Virginia while attending a fair in the Northwest part of the state.
 New MERS-CoV Cases Announced; Over 100 Total Cases Globally
New MERS-CoV Cases Announced; Over 100 Total Cases Globally
29Aug13
The WHO issued a MERS-CoV update yesterday that added 8 additional laboratory-confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV). As noted in the update, “The cases include two men with underlying medical conditions from Riyadh who died, three women and one man, also from Riyadh, and two men from Asir region. Additionally, a previously laboratory-confirmed case from the United Arab Emirates has died.” These 8 cases bring the global lab-confirmed MERS-CoV case count since Sept. 2012 to 102 with 49 fatalities.
The majority of these MERS-CoV cases were reported from the Kingdom of Saudi Arabia (KSA). According to the Saudi Ministry of Health, there have been 84 lab confirmed cases in KSA since Sept. 2012, including 42 deaths (see here).
And just today, the WHO reported an additional two lab-confirmed cases of MERS-CoV in Qatar. Only one of the two cases had traveled abroad and that case had not taken part in Umrah nor visited Al-Masjid an-Nabawi in Medina. These two cases bring the global count of lab-confirmed MERS-CoV cases to 104.
 Setting the Bar for HCV Tx
Setting the Bar for HCV Tx
29Aug13
A NIH-sponsored Phase II clinical trial has demonstrated that a combination of two drugs, Gilead’s sofosbuvir and the old war-horse ribavirin, can provide interferon-free (IFN-free) therapy in a safe and efficacious manner for hepatitis C infections (see NIH press release).
As noted in the press release, ““We saw an overall cure rate of about 70 percent using regimens that did not include interferon,” said Dr. Kottilil. “This is an encouraging result, especially considering the proportion of volunteers who had characteristics — such as being male, having HCV genotype-1 infection, being African-American and having advanced liver damage — that are recognized as predictors of poor response to treatment.”” Genotype-1 HCV is known to be less responsive to IFN therapies and, while other recent trials have also highlighted the possibility of IFN-free regimens, the study participants were largely white. In the present trial, 50/60 participants (all infected with genotype-1 HCV) were African-American. Further, 13 of the participants had liver damage rated as “serious”. Details of the study can be found in the August 28th edition of the Journal of the American Medical Association (here).
As succinctly put by NIAID Director (and study co-author) Anthony Fauci, “There is a pressing need for hepatitis C virus treatments that are less burdensome to the patient, have fewer side effects and take less time to complete. Building on previous work, this trial provides compelling evidence that interferon-free regimens can be safe and effective.” Since 2011, the standard of care for genotype-1 HCV patients has been the use of either of two protease inhibitor [ i.e. telaprevir or boceprevir ] in combination with pegylated-IFN-alpha and ribavirin to treat genotype 1-infected HCV patients.
Sofosbuvir is an inhibitor of the viral NS5B RNA-dependent RNA polymersase. An earlier presentation at the 20th Conference on Retroviruses and Opportunistic Infections (in March of this year) had already shown that “An interferon-free regimen of the direct-acting hepatitis C drugs sofosbuvir (formerly GS-7997), ledipasvir (formerly GS-5885), and ribavirin produced a 12-week post-treatment sustained virological response (SVR12) rate of 100% for both treatment-naive patients and prior non-responders with HCV genotype 1…” Next up for sofosbuvir: IFN- and ribavirin-free regimens in chronic HCV patients, particularly those with HIV co-infection.
There is considerable interest in IFN-free regimens for HCV. As noted in an excellent snapshot of the HCV space in Fierce Biotech [by Decision Resources], the HCV market is expected to grow from about $3B in 2011 to $21B in 2018 before shrinking as the treatment-eligible population in the developed world declines (largely due to preventative measures introduced in the 1990’s such as blood donor screening). That is an enormous market and that means feverish competition. Sofosbuvir and similar “direct-acting antivirals” [DAAs] “…being evaluated in all-oral, IFN-free regimens consisting of one to three DAAs in combinations with and without ribavirin.” The table, at left, summarizes some of the DAAs currently in clinical evaluation.
 Incidence of Lyme Disease 10-Fold Previous Estimates
Incidence of Lyme Disease 10-Fold Previous Estimates
28Aug13
As summarized by the CDC, “Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected blacklegged ticks. Typical symptoms include fever, headache, fatigue, and a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, the heart, and the nervous system.”
Only a small fraction of people bitten by blacklegged ticks develop Lyme disease. However, “Approximately 10 to 20% of patients treated for Lyme disease with a recommended 2–4 week course of antibiotics will have lingering symptoms of fatigue, pain, or joint and muscle aches. In some cases, these can last for more than 6 months. Although often called "chronic Lyme disease," this condition is properly known as "Post-treatment Lyme Disease Syndrome" (PTLDS).” Treatment of PTLDS patients with additional antibiotic regimens is controversial, though most patients are believed to fully recover given enough time. However, others disagree.
Every year, roughly 30,000 cases of Lyme disease are reported to the CDC. But it has been generally understood that this number of cases was an underestimate of the disease’s true incidence. To get a better handle on the actual incidence of Lyme disease, the CDC has been conducting three complementary studies:
• Estimates of the number of people diagnosed with Lyme disease based on medical claims information from a large insurance database.
• Estimates of the number of people who test positive for Lyme disease based on data obtained from a survey of clinical laboratories.
• Estimates of the number of people who report that they’ve been diagnosed with Lyme disease in the previous year, from survey data.
Scientists from the CDC have now presented their preliminary finding at the 13th International Conference on Lyme Borreliosis and other Tick-Borne Diseases (website), held last week in Boston. Their results are summarized on the CDC website (see here). In brief, their preliminary analysis of the data suggests that the number of people infected with Lyme disease each year in the U.S. is about 300,000, or about 10 times the prior estimates. However, the geographical distribution of Lyme disease remains the same in the new studies - 96% of all cases arise in just 13 states: Connecticut, Delaware, Maine, Maryland, Massachusetts, Minnesota, New Hampshire, New Jersey, New York, Pennsylvania, Vermont, Virginia and Wisconsin.
A better measure of the annual incidence of Lyme disease will hopefully lead to greater research, public health policy changes, and increased public awareness.
 Cyclosporiasis Update
Cyclosporiasis Update
21Aug13
The CDC has updated the case count for the cyclosporiasis outbreak in the U.S. For the latest data, please go see this webpage. As of August 20th, a total number of reported cases has risen to 598 distributed among 22 states and NYC. This is up from 400 reported cases on August 1st. No deaths from Cyclospora infections have been reported though for the 456 patients (for whom additional data is available), 40 (~9%) have been hospitalized.
Nebraska and Iowa have conducted an investigation as to the source of the cyclosporiasis outbreak and have reported to the CDC that infections in their states are due to contaminated salad mixes (see the CDC webpage). It is not yet clear if the cases observed in other states is due to the same source.
 Two More Cases of Human H5N1 Infection in Cambodia
Two More Cases of Human H5N1 Infection in Cambodia
19Aug13
Two new cases of human infection by H5N1 influenza have been reported in Cambodia, the 15th ( 9M) and 16th (5F) cases this year. And sadly, the 9M patient has just reportedly died from the infection. To date, 10 of the 16 H5N1 patients in Cambodia this year have died. Since the disease first appeared in Cambodia in 2003, there have been a total of 37 confirmed cases of infection with 29 fatalities. For Cambodia, this is a case fatality rate (CFR) of 78%, one of the highest in the world.
In related news, the outbreak of avian H5N1 in Nepal continues unabated. The government of Nepal has now declared the Bhaktapur district, one of the three districts of the Kathmandu valley, as an emergency zone according to an online article from Bernama, the national news agency of Malaysia. Moreover, "The Ministry of Agriculture has formed a Rapid Response Team to cull some 500,000 fowls in Bhaktapur." In addition, the Indian government has moved to put all states on "bird flu" alert following the avian H5N1 outbreak this month in Chhattisgarh and another outbreak earlier in the year in Bihar.
 H7N9 Update: Suspected New Case in China
H7N9 Update: Suspected New Case in China
09Aug13
A new suspected case of human infection of the H7N9 strain of avian influenza was reported on Friday in south China's Guangdong Province, according to the Xinhua (see here and here), China’s official news agency. The patient, 51F, has tested positive for the virus in testing performed by the Guangdong Provincial Department of Health. Samples have also been forwarded to the Chinese Center for Disease Control and Prevention for confirmation. The patient, who does have a history of exposure to poultry, is in critical condition.
If confirmed, this would be the first confirmed case of human H7N9 infection in the province, thus marking another incremental step in the spread of the virus. This case is most notable not so much because this may be the first confirmed case in humans in almost a month (China is in its inter-seasonal period) but rather for its geographic location. As noted previously on these pages, when H7N9 was first found in avian samples from the province, Guangdong Province is a mere 100 km or so from a major metropolitan center, Hong Kong. A significant portion of past cases arose from another metropolitan center, Shanghai, so the spread to another could lead to significant number of new cases.
In other H7N9 news, a group of biomedical investigators from Jiangsu Province have published a paper in the British Medical Journal describing an instance of probable human-to-human transmission of H7N9 this past Spring. The patient involved form a small cluster with the index case (60M) developing “…a fever, cough, and shortness of breath on 8 March 2013 and was admitted to a Chinese hospital (hospital A) on March 11 with a left upper lobe inflammation.” The patient progressed to the ICU on 15Mar and to a tertiary healthcare facility’s ICU on 18Mar. The patient expired on 04May due to disseminated intravascular coagulation and multi-organ failure.
In the meantime, the index case’s daughter (32F) fell ill on 21Mar and was admitted to the same tertiary facility on 24Mar. She was transferred to the ICU on 28Mar but expired on 24Apr due to multi-organ failure and cardiac arrest. This patient had provided unprotected bedside care to her ailing father up until 18Mar and had no known prior exposure to poultry. From a set of 43 close contacts, only the son-in-law of the index case developed any symptoms of respiratory infection.
Sequencing of viral specimens from the two patients showed that “Sequences of all eight genes of the two strains isolated from patients were nearly identical…”. These and other related observations led the investigators to conclude that: “We believe that the most likely explanation for this family cluster of the two patients with novel avian influenza H7N9 virus infection is that the virus transmitted directly from the index patient to his daughter.”
This conclusion appears to be consistent with the emerging body of H7N9 transmissivity studies performed in ferrets (see the latest contribution, here) and which indicate the virus is capable of limited, though not sustained, human-to-human transmission. But even this limited capability is cause for some concern as it “lowers the bar” for additional mutations that could support sustained human-to-human transmission.
Finally, the reader is referred to two letters published in Nature this week (see here and here). The former correspondence is from Profs. Fouchier and Kawaoka on behalf of 22 biomedical investigators that outlines the set of currently needed experiments to more fully assess the pandemic risk associated with H7N9. These experiments include assessing HA mutations that could enhance transmissibility in humans, NS mutations that could confer resistance to neuraminidase inhibitors, and HA protease cleavage site mutations that enhance viral spread to internal organs. A proposed set of “gain-of-function” experiments is clearly delineated. In the latter correspondence, “The US Department of Health and Human Services (HHS) announces a new review process for certain gain-of-function (GOF) experiments on the avian influenza A (H7N9) virus…”, such as those proposed by Profs. Fouchier and Kawaoka.
 Avian H5N1: Out of Control in Kathmandu?
Avian H5N1: Out of Control in Kathmandu?
07Aug13
Massive outbreaks of H5N1 in bird populations have surfaced since the end of July in Nepal, India, and Vietnam. At the moment, the situation in Nepal seems the most problematic. According to numerous news reports (see, for example, here, here, and here), the outbreak in Nepal has occurred at poultry farms mainly in the Kathmandu valley, though the most recent reports now cite outbreaks in other regions of Nepal. In the past 21 days, there have been 36 confirmed outbreaks in the Kathmandu valley and only 4 outbreaks confirmed outside the valley. Over 50,000 infected fowls have been culled. The current H5N1 outbreak in Nepal is moving very fast.
This follows earlier reports (see here and here) detailing 32 outbreaks of avian H5N1 in Nepal from 11Apr13 to 20May13 that resulted in the deaths of over 122,000 birds, mainly poultry. Interestingly, included in that death toll was a crow found near a custom station at the border with India. This observation may have relevance in the current regional situation (see below).
Perhaps not surprisingly, charges of government failure to contain the outbreak are flying as panic grows in the capital city. The major concerns have been that the government has not moved quickly enough in culling infected poultry to contain the outbreak and that compensation provided to farmers for culled animals is too low, causing farmers to hide infected animals from government inspectors. Most recently, concerns are being raised that the government has been too Kathmandu-centric in its response as avian H5N1 infections crop up outside the valley. The government, which imposed a ban on the import or export of chickens in the Kathmandu valley on August 1st, has responded by stating that its response teams are working around the clock to contain the epidemic. Earlier this week, the Chairman of the Nepal’s Interim Election Council directed government officials to “..control the menace effectively”.
Meanwhile, Nepal is not the only country dealing with an outbreak of H5N1. Earlier this week, the central Indian state of Chhattisgarh issued an alert after an outbreak of H5N1 at a poultry farm at Anjora village. The next day, veterinary officials in India informed the World Organization of Animal Health (OIE) of a second outbreak in Chhattisgarh at a government poultry farm in Jagadalpur where there were 3,600 infected birds and 2,392 deaths from a flock of 6,293. And today, a news report out of Vietnam describes a reoccurrence of bird flu in quails in the Mekong delta province of Tien Giang. In the last month, over 26,000 infected quails have been culled.
Large-scale outbreaks in birds of H5N1 are nothing new, especially since H5N1’a widespread re-emergence in 2003/2004. However, such outbreaks are not without consequence and do warrant rapid action and close scrutiny. There are three major concerns around any large-scale out break of H5N1 (or any other highly pathogenic avian influenza):
1. There are serious socio-economic consequences. As noted by the WHO, “Outbreaks in poultry have seriously impacted livelihoods, the economy and international trade in affected countries.”
2. An increased prevalence of H5N1 in birds, especially those in close proximity to humans, increases the chances of human infection. Since human H5N1 infections yield very high death rates, this is clearly undesirable.
3. An increased prevalence of H5N1 in birds increases the opportunities for viral reassortment and thus the creation of deadly new strains of influenza. For example, new H5N1 strains with enhanced human infectivity or transmissivity would constitute a serious public health issue.
There is already ample evidence that concern #1 is already panning out in Nepal. Concern #2 has yet to manifest itself since there are as yet no confirmed cases of human H5N1 infection in the affected regions. But concern #3 may be the most troublesome. South and SE Asia currently are dealing with ongoing bouts of human infection by the 2009 A/H1N1p pandemic virus, circulating A/H3N2 strains, and a recently quiescent A/H7N9 strain. This boiling cauldron of sub-pandemic strains bears close monitoring due to its capacity to engender new human pandemic strains and epidemic outbreaks of H5N1 in birds only adds to the this capacity.
 Honduras Declares State of Emergency Due to Dengue
Honduras Declares State of Emergency Due to Dengue
01Aug13 Updated 05Aug13
The government of Honduras has declared a state of emergency due to a dengue fever outbreak that has killed 16 people and sickened 12,000, according to news reports out yesterday. In response, the government is making it a priority to control the disease by fighting the mosquitoes that spread it. Already, more than half of Honduras' municipalities have registered dengue fever cases.
Overall, there appears to be many locales reporting much higher case loads of dengue this year. In February, Brazil reported over 200,000 cases in just the first 2 months of 2013, triple last year's case incidence. Roughly half of the cases were caused by the DENV-4 strain of the virus, which was first detected in Brazil in 2011. By July 31, Honduras, Costa Rica, Nicaragua and El Salvador have issued formal alerts. In Guatemala and Panama, officials say they are monitoring the disease, which normally spreads more easily later in the rainy season. The WHO has already noted that, by early July, dengue cases were up some 76% in Central America.
These developments are most striking in the context of recent historical data from the region. The table entitled "Dengue Morbidity and Mortality in the Americas: Honduras, Brazil, and Puerto Rico" (found here), shows the marked growth in dengue incidence over the past decade in the three listed countries. This is clearly a disease spiraling out of control, especially since programs to limit Aedes aegypti, the mosquito vector for the dengue virus, were wound down in the 1970's.
Of particular interest is the observation that Honduras has exhibited a severe disease index ([# of cases of severe dengue / # of total dengue cases] *100) above 10 for each of the past three years and 5 out of the last seven years. Typically, this index is somewhere around 1-3% (see graph, here), though certainly other countries have on occasion exhibited indices above 10. Nevertheless, the scope of new dengue cases in the Americas is in line with the rising global pattern of dengue that places 1/3 of the world's population at risk each year.
There are currently no therapeutics for dengue though a handful of vaccine candidates are under active development. The most advanced of these is a vaccine candidate from Sanofi SA, but clinical trial shortfalls and recent research insights that suggest new directions are needed for in vaccine design [for example, see here and here] may suggest that a safe and effective vaccine is still years away. Compelling action is needed now to mitigate a growing public health crisis.
 Another Worrisome Ort Over Human H7N9
Another Worrisome Ort Over Human H7N9
27Jul13
Human isolates of H7N9 can easily infect human lung tissues and cells, another sign of its pandemic potential, investigators reported today. The investigators are from the University of Hong Kong and their work can be found in the latest edition of The Lancet Respiratory Medicine. In a Perspective published today by CIDRAP, author Lisa Schnirring notes that “Earlier gene studies found markers suggesting that the H7N9 virus has the capacity to infect human respiratory cells, but today's findings are the first to show infection and replication in the lab setting.”
The investigators, led by Dr. J.S. Malik Peiris, examined the ability of a panel of influenza A viruses (including 2 human H7N9 isolates as well as 2009 H1N1p, H5N1, a non-pathogenic duck H7N9 isolate, and a pathogenic H7N7 human isolate) to infect and replicate in a variety of human respiratory tissue types, including “…ex-vivo cultures of the human bronchus, lung, nasopharynx, and tonsil and in-vitro cultures of primary human alveolar epithelial cells and peripheral blood monocyte-derived macrophages.” The study found that “Both human H7N9 viruses replicated efficiently in human bronchus and lung ex-vivo cultures, whereas duck/H7N9 virus failed to replicate in either. Both human A/H7N9 viruses infected both ciliated and non-ciliated human bronchial epithelial cells and replicated to higher titres than did H5N1 (p<0·0001 to 0·0046) and A/Shanghai/1/2013 replicated to higher titres than did H7N7 (p=0·0002—0·01). Both human A H7N9 viruses predominantly infected type II alveolar epithelial cells and alveolar macrophages in the human lung and replicated to higher titres than did H5N1 (p<0·0001 to 0·0078); A/Shanghai/1/2013 replicated to higher titres than did H1N1 (p=0·0052—0·05) and H7N7 (p=0·0031—0·0151). Human H7N9 viruses were less potent inducers of proinflammatory cytokines compared with H5N1 virus.” Human H7N9 isolates were, however, better in vitro proinflammatory cytokine inducers than H1N1p.
In an accompanying Commentary, Jessica Belser and Terrence Tumpey (both at the CDC) place these finding in the context of recent ferret studies. These latter have shown that human isolates of H7N9 are capable of efficient transmission via direct contact and, to a lessor extent, via respiratory droplets. They note the interesting observation that while H5N1 can efficiently replicate in many cell/tissue types of the ferret airway and can cause severe disease in humans, H5N1 does not transmit efficiently in ferrets even via direct contact. They rightly point to the unique characteristic of the H7N9 hemagglutinin (HA) in which H7N9 HA seems ideally optimized to bind both avian receptors (alpha 2,3-linked sialic acid) and human receptors (alpha 2,6-linked sialic acid).
Belser and Tumpey note that “….the study by Chan and colleagues raises as many questions regarding the pathogenicity of H7N9 viruses as it addresses.” Besides the still unsubstantive case for a source of human infection, the unusual age-distribution in confirmed cases, the mechanism(s) by which H7N9 (and perhaps Eurasian-lineage H7 viruses in general) evade engagement of the host innate immune system, and the surprising lack of conjunctivitis among human H7N9 cases (in stark contrast to other human H7 influenza infections) all require better explanation.
As always, the interplay between viral tropism, receptor binding specificities, host cellular immune naiveté, the magnitude of local innate immune responses, and viral transmissivity help define the pandemic character of a given virus and differentiate it from its viral cousins. For H7N9, the ongoing “summer of assessment” has so far only increased concerns that, should the virus return this fall, it may well be a dangerous second encounter.
 A Sudden Burst of Cyclosporiasis in the U.S.
A Sudden Burst of Cyclosporiasis in the U.S.
27Jul13
It all began in late June when the CDC was notified of 2 laboratory-confirmed cases of a rare (in the U.S.) food-borne infection in Iowa. The offending pathogen is known as Cyclospora cayetanensis, a protazoa that causes prolonged diarrheal illness, often in patients with a history of recent travel to Cyclospora-endemic areas. By July 25th, the CDC had been notified of a whopping 321 cases spread across multiple states (see case map, below), with most of the designated “onset dates” ranging from mid-June through early July (see timeline, below). At least 18 people were reportedly hospitalized in three different states.
What is so surprising about this outbreak is the sheer number of cases reported, magnitudes reminiscent of previous large outbreaks in the U.S. during 1996 and 1997. In those years, well over 1000 cases were reported. In a detailed study entitled “Laboratory-Confirmed Sporadic Cases of Cyclosporiasis --- United States, 1997—2008” the CDC analyzed accumulated data over a 12 year period. This study found that, of the aggregate 1,110 sporadic (non-outbreak) cases reported to the CDC in those 12 years, “The annual number of reported cases varied (median: 98 cases; range: 14--148); the population-adjusted incidence rates (number of cases per 100,000 persons) ranged from a low of 0.01 in 1997 to a high of 0.07 in 2002”. Approximately 3,000 outbreak-associated cases were reported for the same period and, in the case of outbreaks, the average number of outbreak-associated cases varied greatly (range: 0--1,448 for outbreak-associated cases). Thus, the number of reported cases in just the past 6 weeks is already well above recent historical averages for sporadic cases in the U.S. and is more reminiscent of an “outbreak” year.
The geo-distribution this year (so far) is also unusual. For sporadic cases during the 1997-2008 period, 498 (44.9%) were in residents of Florida (228 cases), NYC (200 cases), or elsewhere in New York state (70 cases), and >50 cases were reported by each of five other states (Connecticut, Georgia, Massachusetts, New Jersey, and Pennsylvania). Thus, sporadic cases have been largely an event of the Eastern and Southeastern U.S. The case map for this year is clearly very different (see below).
According to the CDC, “The parasite Cyclospora cayetanensis is a unicellular, coccidian parasite transmitted by ingestion of infective oocysts (e.g., through contaminated food or water). The most common symptom is watery diarrhea. Although humans are the only known hosts of this Cyclospora species, direct person-to-person transmission is unlikely; the oocysts shed in feces require days to weeks under favorable environmental conditions to become infective. The need for Cyclospora oocysts to survive long enough both to sporulate and subsequently to be ingested by a susceptible person suggests that the oocysts are quite hardy and unlikely to be killed by routine chemical disinfection or sanitizing methods used for food or water. The incubation period averages 1 week (range: ~2--14 days). Infection responds to treatment with trimethoprim-sulfamethoxazole, but untreated persons can have prolonged illness, with remitting-relapsing symptoms, for several weeks or months.”
Cyclosporiasis is most common in tropical and sub-tropical regions. The earliest reports of cases of cyclosporiasis occurred in the late 1970’s out of Papua New Guinea. However, in any given year, only roughly 1/3 of reported cases are associated with recent international travel to/from endemic areas while another 1/3 are domestic cases with no known international travel.
The CDC is, as yet, unsure of the food source(s) of this outbreak (though prior outbreaks have had imported fresh produce implicated as the contaminated source) nor is it clear that all cases in all states are part of the same outbreak. There have not been any common events identified among the case patients.
Cases of Cyclosporiasis in US (as of Aug. 1, 2013) - A total of 400 cases of Cyclospora infection have been reported from 16 states and 1 city. The number of cases identified in each area is as follows: Iowa (146), Texas (113), Nebraska (81), Florida (25), Wisconsin (9), New York City (5)†, Georgia (4), Illinois (4)†, Arkansas (2), Kansas (2)‡, Louisiana(2)†, Missouri (2)†, Connecticut (1), Minnesota (1), New Jersey (1), New York (1)†, and Ohio (1).
† Includes one case that was likely acquired out of state.
‡ Includes two cases that were likely acquired out of state.
FIGURE & LEGEND CREDIT: CDC
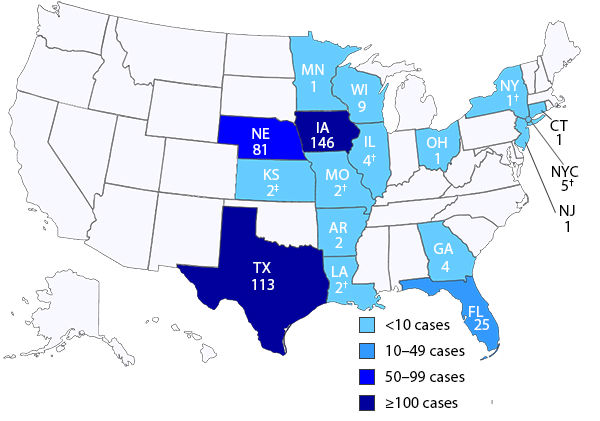
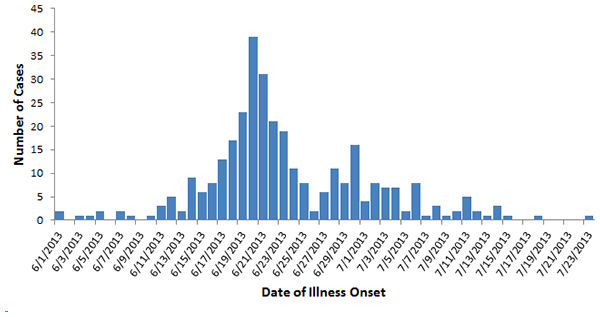
Timeline, Confirmed Cyclosporiasis Cases, United States, June—July 2013 (N=325)*
Data are current as of 5pm EDT, 8/1/13. Data are preliminary and subject to change. Cases reported to CDC as of 5pm on 8/1/13 for which onset of illness dates were available. A case is defined as laboratory-confirmed Cyclospora infection in a person with onset of illness in June or July 2013 and no known travel outside of the United States and Canada in the 14 days before onset of illness. It is not yet known whether all reported cases are part of the same outbreak.
FIGURE & LEGEND CREDIT: CDC
 A New Case of A/H7N9 Influenza in China - New Province
A New Case of A/H7N9 Influenza in China - New Province
21Jul13
The Chinese government has reported the first new case of confirmed H7N9 infection in humans since May of this year. The patient (61F), a resident of Hebei Province in north China, began to experience symptoms on July 10th and admitted to the hospital with severe pneumonia on July 14th. When her condition did not improve, she was transferred to the ICU on July 18th. A diagnosis of H7N9 infection was confirmed on July 20th. The patient is currently in critical condition in a Beijing hospital. The patient reportedly had contact via shopping at a live market that also sold live poultry. This latest case raises the global case count to 134 confirmed cases with 43 fatalities and represents the first case of human H7N9 infection reported in the Province.
In addition, a new study, published this past week in the journal Science, reports that H7N9 isolates, obtained from more than 10,000 samples from poultry markets, poultry farms, wild bird habitats, and poultry and swine slaughterhouses across China from March to May this year, were compared genetically and experimentally to H7N9 from human isolates.
Out of the 10,000+ field samples, the investigators were able to identify 52 that were positive for H7N9. Of these, 50 were from live market samples. 37 of the 52 samples were propagated in eggs and compared to 5 isolates obtained from infected humans. While the sequences were all very similar, once again the human isolates showed important markers of human adaptation. Only virus from human isolates was able to cause disease in mice and ferrets, including weight loss. And perhaps most importantly, while 4/5 human isolates were able to transmit virus via direct contact, the 5th isolate was able to efficiently transfer virus via respiratory droplets. This latter point suggests that at least some viral species do exist that are capable of efficient human-to-human transmission.
Earlier in the week, Dr. Robert Webster and colleagues published a paper in mBio demonstrating that the viral isolate from the first confirmed clinical case of H7N9 (the A/Shanghai/1/2013 isolate) was in fact a mixture containing 65% Arg-bearing and 35% lysine-bearing at position 292 in the viral neuraminidase. Importantly, while the isolate mixture displayed a phenotype of sensitivity for the three major neuraminidase inhhibitors ( oseltamivir, peramivir, and zanamivir ), the plaque-purified R292 species was highly resistant. Thus, standard assays for resistance to neuraminidase inhibitors in clinical isolates may mask the presence of resistant forms if the clinical isolate is in fact a mixed population of sensitive and resistant species, even if the sensitive form is the minor component in the mixture. This is a critical and worrisome observation. As noted by the authors, "The neuraminidase (NA) inhibitors oseltamivir and zanamivir are currently the front-line therapeutic options against the novel H7N9 influenza viruses, which possess an S31N mutation that confers resistance to the M2 ion channel blockers." Lack of therapeutic efficacy for neuraminidase inhibitors would leave the world essentially defenseless in a large outbreak of H7N9 in humans.
Finally, a bit of happy news this past week. A 25F patient from Jiangsu Province, diagnosed with H7N9 infection back on April 8th, gave birth to a healthy baby girl. The mother eventually recovered from H7N9 in May, but remained under care during the final months of her term. Mom and baby are both reportedly doing fine.
 Prevnar-7’s Progressive Impact
Prevnar-7’s Progressive Impact
21Jul13
A recent paper, published in The New England Journal of Medicine, quantifies the dramatic impact of Prevnar-7, the vaccine against Streptococcus pneumoniae, and seeks to assess whether initial successes were sustained over the past decade.
The question is important since a potential concern is that, with Prevnar’s success, the door would open for other non-vaccine strains of S. pneumoniae (“serotype replacement”) or even other bacterial species to “take over the territory” and cause disease that would blunt the beneficial impact of vaccine. In other words, what bacteria will wind up colonizing our nasopharyngeal passages if not the seven S. pneumoniae strains covered by the vaccine?
As stated in the paper, “The introduction of the 7-valent pneumococcal conjugate vaccine (PCV7) into the U.S. infant immunization schedule in 2000 resulted in major reductions in the incidence of invasive pneumococcal disease in all age groups.” One remarkable thing about Prevnar-7 is that its protective effects extended outside the age group actively receiving immunizations, an example of “herd immunity”. A study published in 2006 found that vaccination with Prevnar-7 prevented 800,000 hospitalizations for pneumococcal pneumonia in the U.S. alone. The current study extends this analysis through 2009, prior to any impact from the “next generation” pneumococcal vaccine, Prevnar-13. The current study compares hospitalization rates over three time periods: 1997-1999 (before Prevnar-7), 2001-2006 (early Prevnar-7 years, and 2007-2009 (late Prevnar-7 years).
Over this time span, “…there were 17,892,085 hospitalizations for pneumonia, representing 4.1% of all U.S. hospitalizations other than those for childbirth, including 7.2% of hospitalizations among children and 3.9% of hospitalizations among adults.” And, “Annual rates of hospitalization for pneumonia were highest at the extreme ends of the age spectrum in all 3-year periods, with rates for children younger than 2 years of age similar to those for adults 65 to 74 years of age, at approximately 1000 hospitalizations per 100,000 persons. Rates for persons 75 years of age or older were two to five times as high.”
The results shows that continued immunization with Prevnar-7 through 2009 resulted in deeper reductions in the average annual rates of hospitalizations for pneumonia in the U.S. The results were most notable for the age groups at the extremes of the range. Overall, the authors estimate an age-adjusted annual reduction of 54.8 per 100,000 cases, which translates to 168,000 fewer hospitalizations for pneumonia annually. 47,000 of these fewer hospitalization are found in children less than 2 years of age (the group that is actively immunized) while 73,000 fewer hospitalizations occur annually in the 85+ age group (where there is no routine immunization occurring). There was no significant impact in the age-ranges of 5-17 and 18-39 years.
The authors also found that “Seven years after the introduction of PCV7, invasive pneumococcal disease caused by vaccine serotypes was almost eliminated in children younger than 5 years of age and declined by more than 85% in all unvaccinated age groups.” It is important to note that unvaccinated age groups still retain a substantial residual disease burden for invasive pneumococcal disease. It remains to be seen whether the advent of Prevnar-13 leads to additional reductions and in which age groups.
However, serotype replacement remains a real concern. First noted in 2005 by the CDC [ref1], use of surveillance data now clearly show increased circulation of non-vaccine serotypes 1, 3, 6A, 6C, 7 F and 19A in countries with routine vaccination (ref2). And as first noted by the CDC study, some serotypes, such as 19A, are increasingly drug resistant. Replacement serotypes are important considerations because, as noted in ref2, “The direct and indirect costs associated with pneumococcal disease are high, thus herd protection and infections caused by non-vaccine serotypes both have strong effects on the cost effectiveness of pneumococcal vaccination. Recent evaluations highlight the public health significance of indirect benefits, prevention of pneumonia and AOM [acute otitis media] and coverage of non-PCV7 serotypes by higher valency vaccines.”
 Another Confirmed H5N1 Human Case in Cambodia
Another Confirmed H5N1 Human Case in Cambodia
12Jul13
A joint statement from the WHO and the Cambodian Health Ministry reports the 14th human case of H5N1 this year, according to a news report from Xinhua, China’s official news agency. The patient, 3M, was admitted to hospital last Monday with fever, dyspnea, and cough. He is currently in stable condition.
In other H5N1 news, a group of Chinese researchers have shown that “..pigs are naturally infected with avian H5N1 virus and highlight the potential threat to public health due to adaption or reassortment of H5N1 virus in this species.”
 Mumps Outbreak in Wales: Waning MMR Protection?
Mumps Outbreak in Wales: Waning MMR Protection?
09Jul13
The trivalent MMR vaccine is a stalwart of modern health case, conveying lifelong immunity from measles, mumps, and rubella, especially if the patient receives both of the recommended jabs. A recent article on FierceVaccines by Nick Paul Taylor, citing a report appearing in The Guardian, describes a growing body of data suggesting that while the vaccine works well for measles and rubella, mumps may be another matter.
In the first quarter of 2013, the U.K.’s National Health Service reported 948 cases of mumps versus 673 measles cases, numbers that prompted a national effort to increase the uptake of the vaccine. But half of the reported mumps cases were in individuals who had received at least one jab with MMR. As a result, Public Health England reports that "…some waning immunity may be contributing to transmission." The idea that the protective effects of the vaccine may abate over time is not new for mumps (see, for example, here and here). Exacerbating matters are possible antigenic differences between the vaccine strain and outbreak strains that crop up from time to time (ref1). Moreover, the recent resurgence of mumps in the U.S. and Canada sometimes occurred in the context of high 2-dose vaccination coverage and thus raised the question of the vaccines durable response (ref2).
Vaccination rates with MMR have been under steady pressure over the past decades due, in part, to the now fully discredited theory linking autism and other disorders to the vaccine. Falling vaccination rates are a concern since, if vaccination uptake in the population is not sufficient to maintain herd immunity, vaccination becomes the only means to protect a given individual. And for children who have received only a single round of vaccine, this can be problematic (see this report).
Mumps is a highly contagious, self-limiting viral disease spread through contact with respiratory droplets from an infected person or by sharing food or drink. Prior to introduction in 1967 of the vaccine, mumps was the leading cause of viral meningoencephalitis in the United States, though the actual rate of encephalitis was rare (<2 per 100,000). Typically mumps presents with swollen glands, fever, vomiting, and headache. The disease is typically not severe in children, but older individuals can experience painful orchitis or oophoritis and are at risk for long-term fertility complications.
Thus, mumps joins other vaccine-preventable diseases, such as pertussis (ref3; ref4), TB (ref5), and polio (ref6) that have displayed characteristics of waning long-term protection. As noted in The Guardian article, solving the problem of waning protection can be a knotty one, not easily solved. And in the end, these observations point to limitations in our understanding of long-term T- and B-cell immune memory.
 MERS-CoV Confirmed Cases Hits 80 with 42 Deaths
MERS-CoV Confirmed Cases Hits 80 with 42 Deaths
05Jul13
The SARS-like corona virus, MERS-CoV, continues to exert its influence on the global stage. The current global count of lab-confirmed cases of human infection with the virus now stands at 80, up from 60 just a few weeks ago. A total of 43 fatalities amongst the 80 confirmed cases have occurred. A complete listing of cases can be found at Sharon Sanders' excellent webpage. The latest WHO update has been published on Friday.
A new study just appeared in the The Lancet that examines the pandemic potential of MERS-CoV as compared to pre-pandemic SARS. Importantly, the study concludes "that MERS-CoV does not yet have pandemic potential." But extreme caution are still the watch words, as one should not over-interpret these results. This study cannot predict the future behavior of the MERS-CoV virus, including potential viral mutations.
In the meantime, the WHO has convened an emergency committee to assess the dangers that MERS-CoV presents to the international community, according to CBS News. " A spokesperson for the WHO told CBSNews.com that the emergency committee is part of the International Health Regulations (IHR) that were put in place in 2007. The IHR Emergency Committee consists of international experts who will advise the WHO Director-General when the medical issue becomes a "public health emergency of international concern." They also advise on temporary recommendations for travel, surveillance, clinical management, infection control." The Committee last met in 2009 over the H1N1p pandemic.
Any virus, such as MERS-CoV, that infects humans with a CFR north of 50% (see this reference) is worthy of close scrutiny and mindful preparation, just as the WHO and CDC are doing.
 H5N1 Claims Another in Cambodia
H5N1 Claims Another in Cambodia
05Jul13
Cambodia has reported its 13th case of influenza A/H5N1 this year. Sadly, the 6F patient died from the infection on Jun 28th, after falling ill on Jun. 24th. A total of 9 of the 13 confirmed cases this year in Cambodia have been fatal. Since 2003, there have been a total of 34 confirmed cases of H5N1 in Cambodia.
Of potential interest, an Indonesian news report is noting the alarmingly sudden deaths of thousands of chickens, ducks, and entog in the village of Cikalahang, Dukupuntang district. Bird flu, possibly H5N1 is suspected.
 Another First – Influenza A/H6N1 Infection in Humans
Another First – Influenza A/H6N1 Infection in Humans
28Jun13
There has been a rash of recent firsts in the infectious disease world. Late last year MERS-CoV was noticed on the scene, just as a new set of H3N2v swine influenza infections was making its way through the US. Early this year we had the first-ever major outbreak of a H7N9 influenza in humans. Now, another: the first documented case of influenza A/H6N1 in humans.
The 20F patient was hospitalized on May 5th for mild pneumonia, treated with neuraminidase inhibitors, recovered, and was released from hospital on May 11th. The case was reported to CDC-Taiwan on May 20th. Subsequently, whole genome sequencing efforts by the CDC-Taiwan identified the virus as A/H6N1, typically a low pathogenicity virus broadly found in birds such as chickens. The patient had no history of contact with poultry and had not traveled abroad.
The Taiwan CDC has released full sequence of the virus. However, as noted by Recombinomics, the sequences from the human isolate were more closely related to recent healthy chicken sequences obtained by Taiwan’s Animal Health Research Institute. Importantly, sequences from both sources showed key features in the viral hemagglutinin consistent with enhanced binding to mammalian receptors. These included the E189V and G228S mutations in the receptor binding site and the absence of an N-glycosylation site at position 158. However, N-glycosylation corresponding to position 158 is more typical of seasonal human flu virus than avian influenzas [ see this link]. The H6 HA from the human isolate contains 7-8 potential sites of N-glycosylation (at positions 26/27, 39, 183, 307, 312, 499, and 558; numbering from Met1) that correspond to the number and position of N-glycosylation sites typically found in H6 viruses.
Indeed, the HA sequences of the human isolate and the latest chicken isolate are virtually identical to each other. Two notable exceptions to this identity are the presence of P200L and A301T in the human isolate. For the former mutation, inspection of all 42 chicken isolates of H6N1 from Taiwan in GISAID shows the invariant presence of P200. For the latter mutation, mutations at this position are seen in the ensemble of chicken sequences, but typically as A301V or A301E.
Recombinomics concludes: “The presence of G228S is of concern because it was present in H2N2 in the 1957 pandemic as well as H3N2 in the 1968 pandemic and it was introduce in H5 sequences used in transmission studies. Q226L was also in the H2N2 and H3N2 pandemic sequences, as well as H7N9 sequences in human cases in the Shanghai area, and a traveler to Taiwan (represented by A/Taiwan/1/2013). “ It may be anticipated that if H6 viruses were to pick up the Q226L mutation, an increase in human transmissivity would result.
There have been no further reported cases of human H6N1 infection in Taiwan or elsewhere since this index case. Interestingly, 36 close contacts of the patient were monitored for signs of infection and four of them developed flu-like symptoms, though later testing failed to identify H6N1. H6 influenza viruses were first isolated in Turkey in 1965 and have subsequently been found widely in avian species. A study published in 2008 demonstrated that H6 influenza viruses can infect ferrets and mice productively, suggesting at the time that human infection by H6 viruses was certainly possible. Moreover, these authors were motivated, in part, by the observation the “An H6 influenza virus was identified as a potential progenitor of the H5N1 viruses that emerged in Hong Kong in 1997.” An actual case of human H6N1 infection thereby promotes the possibility of an H6 epidemic or pandemic, though the possibility is clearly still remote.

H7N9 Update - Week 24
15Jun13
No additional confirmed cases of human H7N9 infection have been reported since early May. However, The Lancet is now reporting the case of a 15M from Jiangsu province who was co-infected with A/H7N9 and a seasonal A/H3N2 viruses. The patient presented on April 25th and was admitted to hospital the next day, receiving oseltamivir therapy. The patient recovered and was discharged on May 2nd. The case is of interest for several reasons:
1. It is the first documented case of influenza virus co-infection involving H7N9. Co-infection of two influenza A viruses could result in reassortant viruses. Reassortants could possess new characteristics of transmission, virulence, and Tamiflu (oseltamivir) susceptibility. Co-infections involving 2 influenza A viruses have been documented rarely and the rate of co-infection of two influenza A viruses has been estimated to be 1-3%.
2. The case does not appear to have been previously listed by either the Chinese government or the WHO.
3. The date of onset places this case near the end of the train in terms of reported cases from China. It is interesting to note that other cases with proximal onset dates (after 15-Apr) also were more mild cases or led to rapid recovery.
Not withstanding this case, there is otherwise no news of additional infections or expanded geographical dissemination. Unfortunately, one additional death has been reported (case #19) but, in other good news, there are now only 14 patients remaining hospitalized. The Chinese government is now moving to monthly updates on H7N9, on the 10th of each month.
Two groups have now reported the successful generation and testing of H7N9 vaccines: a group from Medicago with a VLP-based vaccine candidate and, more recently, a team including Inovio Pharmaceuticals. This latest candidate is a DNA vaccine that “…achieved greater than 1:40 hemagglutination inhibition (HAI) in 100% of tested animals (n=10), with a geometric mean HAI titer of 1:130 against the A/Anhui/1/13 strain of H7N9 virus. HAI titers at or above 1:40 are considered to denote protection against the influenza virus in humans.” Notably, the vaccine candidate was “…was designed, optimized, and manufactured within two weeks.” Meanwhile, traditional influenza vaccine production efforts in chicken eggs are off to their usual challenging course [see Link_1 and Link_2].
Finally, the reader is referred to an outstanding Perspective that has just appeared in the New England Journal of Medicine from David Morens, Jeffery Taubenberger, and Anthony Fauci. The article is a great summary of the current H7N9 situation.
 2009 H1N1pdm: Still Making Noise
2009 H1N1pdm: Still Making Noise
16Jun13
The influenza season in the Southern Hemisphere looks to be ramping up and, with it, marked outbreaks of the 2009 H1N1p virus (a.k.a. H1N1 swine flu). While this virus played only a minor role in the just past influenza season in North America and Europe (where H3N2 was more dominant), it was concurrently a particular problem in South and SE Asia, especially in India. And with the coming season in the Southern Hemisphere, it is already making its presence felt.
This is especially true in South America and portions of the Caribbean. According to the most recent report from PAHO, South America is already seeing high rates of acute respiratory infections (though not outside of known ranges for this time of year). RSV infections are predominant in many countries, except for Brazil where H1N1p predominates. There appears to be a bifurcation in terms of which respiratory viruses are in co-circulation: with RSV and H3N2 co-circulating in Bolivia, Ecuador, and Peru while H1N1p is co-circulating in Argentina, Columbia, Venezuela, and Chile.
Another report tells of over 200 deaths to date this year in South America due to H1N1p. Venezuela appears to be in the “ascent phase of an epidemic outbreak” of 2009 H1N1p according to another article published in The Universal last Thursday. According to this article, 414 new cases of 2009 H1N1p were reported in just the past week and bringing the cumulative total of confirmed cases to 1,138. The number of A/H3N2 infections for the year also increased to 129. Citing data from the Weekly Epidemiological Bulletin No. 22, published by the Ministry of Popular Power for Health, the ILI index nearly doubled over the past week (to 1,026) and severe acute respiratory infections also increased from 310 cases the week preceding to 466 this past week, both of these against a backdrop of ~20% week-over-week increases in pneumonia and acute respiratory infections. At least 4 have died from H1N1 this past week. According to another report, “The current outbreak has surpassed one in 2011 that resulted in 900 cases and eight deaths.” And yet another report notes “Venezuela's doctors' union is warning of a possible resurgence of swine flu in the country and is reporting at least four new deaths this week. “ These most recent data appear consistent with an earlier report at the end of last month citing 250 human 2009 H1N1p infections and 17 deaths. The H1N1p virus is also making its presence felt in Argentina where “So far, 12 people have died from A/H1N1 in Argentina, including seven in the province of Buenos Aires and one in the northeastern province of Santa Fe.”
Meanwhile, in SE Asia, Vietnam has reported its third H1N1p fatality in the past week (its fourth since April).
The pH1N1 influenza virus continues to remind us that it is still a dangerous pathogen and perhaps not quite ready to be relegated to mere “seasonal flu” status. Sequence information on the influenza virus from clinical isolates from South America are needed to ascertain if the virus has undergone further genetic alterations.
 Confirmed MERS-CoV Cases Pass 60 with 34 Deaths
Confirmed MERS-CoV Cases Pass 60 with 34 Deaths
14Jun13
The WHO today issued a Global Alert and Response (GAR) raising the official number of confirmed cases of human infection by the SARS-Like MERS-CoV virus to 58 with 33 fatalities. But additional news releases during the day immediately added to the count, raising the total number of confirmed cases to 61 with 34 fatalities. A significant number (46) of these cases have been reported from the Kingdom of Saudi Arabia [KSA]. A breakdown of the confirmed cases by reporting country can be found on the CDC website. A more detailed confirmed case list by Sharon Sanders can be found at this web page.
In related news, 4 additional genomic sequences from MERS-CoV isolates (all from the Al-Hasa region of KSA) have now been deposited in GenBank. This brings to nine as the total number of complete sequences of MERS-CoV isolates published to date. A detailed analysis of these nine sequences can be found at this web page, published by the Andrew Rambaut, Institute of Evolutionary Biology, University of Edinburgh. Of particular interest is the suggestion from this analysis that the recent viral isolates from KSA “…represent an emerging cluster of human-circulating cases with a common ancestor in the second half of 2012, meaning the trees above might represent 3 independent jumps [to humans from an as yet unidentified zoonotic reservoir].” As recently noted by Recombinomics, these sequences “… fully support human transmission of the novel coronavirus in the Middle East, as well as evolution via homologous recombination.”
Finally, CIDRAP, reporting on a CDC conference call yesterday with clinicians, noted “..that more than 30 US patients have been tested for MERS-CoV…”, all of them negative for the virus. It remains unclear how the testing was performed. The CDC “… is advising clinicians to consider MERS-CoV in patients who have an unexplained, acute respiratory illness, which may include fever or cough, with suspected pneumonia and a history of travel from the Arabian Peninsula or neighboring countries within the past 14 days.”
 MERS-CoV (hCoV-EMC) Spreads to Italy; 30 Deaths Globally
MERS-CoV (hCoV-EMC) Spreads to Italy; 30 Deaths Globally
03Jun13
Five new cases of confirmed infection with the novel SARS-like virus, hCoV-EMC (now MERS-CoV), occurred over the weekend, three of them, for the first time, in Italy. The Italian index case (45M) recently spent 40 days in Jordan with his son, a resident of the latter country, and a suspect case himself. The patient was hospitalized on May 28th after returning to Italy on the 25th. He is in stable condition. The two other cases in Italy (2F and 42F) are close contacts of the Italian index case (daughter and colleague, respectively). They too are in stable condition. Italy is the eighth country to report confirmed cases of MERS-CoV. The Kingdom of Saudi Arabia also reported three deaths over the weekend and a new case on Monday.
These cases bring the global count to 54 confirmed cases since September of last year with 30 fatalities. For a complete listing of all cases, see Sharon Sander's comprehensive table at FluTrackers.com.
As noted by Recombinomics, "The increase in [MERS-CoV] exports has been dramatic with confirmed or suspect cases imported into France, Tunisia, Morocco, and Italy (all by commercial airline). None of the exporting countries (UAE, Qatar, Jordan) have reported a case identified by surveillance." Current surveillance efforts do not comprise a winning strategy to contain global dissemination.
 H7N9 Puts on the Brakes in China
H7N9 Puts on the Brakes in China
17May13
The number of confirmed cases of H7N9 influenza in China remains at 130 with one additional case in Taiwan, giving a global total of confirmed human infections of 131. In other related news of interest:
1. The Chinese province of Zhejiang ended its Level IV Emergency Response yesterday in light of the fact that there have been no new human cases of H7N9 in the past 28 days. Today, two other provinces followed suit: Shandong and Jiangsu. There have been no new human infections reported for 21 days in either province. The municipality of Shanghai had previously ended its emergency response on May 10. Medical observation of close contacts of infected patients has also ended.
2. The first patient reportedly infected in Shandong province was discharged from the hospital yesterday. The patient was case #103 in the listing table.
3. An article appeared yesterday suggesting that the recent warm weather in China is playing a part in the sudden attenuation of the H7N9 outbreak.
4. A paper published yesterday in Eurosurveillance investigated the association in the Chinese province of Zhejiang between exposure to poultry and human H7N9 infection. In brief, the paper finds that, of the 12 studied cases of human infection, all had a prior history of direct exposure to poultry or live poultry markets. In addition, viral RNA was detected in all poultry markets frequented by the infected human subjects. From a total of 135 samples obtained from the markets, 38 tested positive for H7N9. In addition, viral RNA was detected in and around the domiciles of two of the cases. The investigators also tested 339 throat swabs (but not sputum samples) from the close contacts of the patients but none tested positive for H7N9. Interestingly, only a few (4) poultry vendors were infected with the virus. It remains unclear why most vendors remain infection free despite purportedly frequent exposure to infected poultry. Finally, after closure of the markets, the investigators noted that there were no additional cases of human infection, hence suggesting an epidemiological link and an infection source.
5. Exports of poultry and poultry related products have been halted out of a farm in the Chinese province of Guangdong after H7N9 was detected in a nearby market. Confirmation of H7N9 in the market sample would mark only the second time the virus has been detected in the province in poultry, the first occurring last month. Guangdong Province has had no reported cases of human infection by H7N9, but nonetheless has been a point of concern due to its proximity to Hong Kong.
6. Using synthetic biology to re-create the H7N9 virus from its genetic sequences, J Craig Venter and Novartis have teamed up to create a vaccine in less than one week, according to an article in The Boston Globe. The scientists used a library of flu genes already known, selected certain library entries, and edited them, including synthesis of H7N9-specific sequences, to create the entire H7N9 viral genome. The work was just published in Science Translational Medicine. “After receiving details of its genetic code on Easter Sunday, the researchers were able to synthesize the virus by the following Tuesday and determine the best design for a vaccine by that Saturday.” Impressive and hopefully immunogenic.
 H1N1p Flu Outbreak in Venezuela Claims 17
H1N1p Flu Outbreak in Venezuela Claims 17
28May13
An outbreak of 2009 H1N1p has infected some 250 people and killed 17 in Venezuela, according to a report by Reuters and citing media and local authorities. Most of the cases Most of the cases were reportedly in border states near Colombia, but the Venezuelan government has yet to confirm anything yet.
 A/H7N9 Influenza Update
A/H7N9 Influenza Update
13Jul13
The Chinese government has provided an update on the status of H7N9 cases. The National Health and Family Planning Commission announced last Wednesday that the official confirmed case count now stands at 132 with 43 fatalities and 4 patients remaining under care. With the additional reported case in Taiwan, the global case count now stands at 133. The CFR for A/H7N9 now stands at 33%.
Concerns about the immunogenicity of H7N9 in humans, and hence the ability to create an effective vaccine, have been allayed at bit by news from the vaccine front. Inovio Pharmaceuticals announced (see this news report) the results of a preclinical challenge study against H7N9. The company’s DNA vaccine, which encodes the sequence of the viral HA gene, conferred 100% protection to vaccinated mice. Also last week, Novavax, Inc. announced commencement of a Phase I clinical trial to test their H7N9 VLP-based vaccine [see this news report]. “This Phase 1, randomized, observer-blinded, placebo-controlled trial will enroll up to 280 eligible adults. Each subject will be randomized into one of seven treatment groups, including placebo, or varying doses of the A(H7N9) vaccine, with or without an adjuvant. Each subject will receive two identical intramuscular doses at Day 0 and Day 21 and undergo study follow-up for approximately one year after the second dose. All subjects will be evaluated for safety and immunogenicity.”
In other news, a new study, published yesterday in the journal The Lancet, is a comparative epidemiological evaluation of laboratory confirmed cases of H7N9 and H5N1 in China. Among other findings of interest, it was observed that the fatality risk on admission to the hospital was 36% for H7N9 versus 70% for H5N1. H5N1 remains the king of deadly avian influenzas.
A new conundrum has popped up. In a letter to the journal Emerging Microbes & Infections, CDC-Shanghai investigators reported striking differences between pediatric and adult cases of H7N9. During the period from early April to late May, Shanghai’s Sentinel Surveillance System for Influenza-like Illness identified 2 H7N9 cases by RT-PCR, out of 1799 screened suspect patients. Both cases were in boys less than four years of age. In contrast, 17 adult H7N9 infected cases were reported by April 10 to the Surveillance System for Pneumonia of Unexplained Origin. The severity of infection was directly linked to lymphopenia (like measles), age, and radiological pathology of the chest. In short, mild H7N9 infections were not common in Shanghai but those that were found were demonstrably milder. On the other hand, examination of all known cases has illuminated a number of “mild cases”, occurring even in adults, leading to the theory that some sort of sustained human-to-human transmission must be occurring, possibly through asymptomatic cases especially in the young.
In apparent support of this concept, two major papers appeared this week in the journal Nature on the pathogenesis and transmissivity of H7N9 in animals, including pigs and ferrets: one by Kawaoka and colleagues in Japan and the US (here) and the other from Terrence Tumpey’s lab at the CDC (here).
In the former paper, three different H7N9 strains from human isolates were studied in mice, ferrets, and non-human primates and compared to the 2009 H1N1p virus. In brief, the H7N9 viruses were more pathogenic in mice than H1N1p and a control avian H7N9 virus. In non-human primates, both the H7N9 and the non-pathogenic H7N9 control replicated well in both the upper and lower respiratory tracts. All the H7N9 viruses replicated well in the upper respiratory tract of ferrets and one of the pathogenic H7N9 viruses was able to support transmission in ferrets through respiratory droplets, though not well.
In the latter paper, two H7N9 viral specimens, isolated from fatal human cases, were evaluated for their ability to cause disease in mice and ferrets as well as to transmit virus to disease-naïve animals. “Both H7N9 viruses replicated to higher titre in human airway epithelial cells and in the respiratory tract of ferrets compared to a seasonal H3N2 virus. Moreover, the H7N9 viruses showed greater infectivity and lethality in mice compared to genetically related H7N9 and H9N2 viruses. The H7N9 viruses were readily transmitted to naive ferrets through direct contact but, unlike the seasonal H3N2 virus, did not transmit readily by respiratory droplets. The lack of efficient respiratory droplet transmission was corroborated by low receptor-binding specificity for human-like α2,6-linked sialosides.”
Despite some difference in the results of the two reports (e.g. over the ability of H7N9 virus to bind to (alpha-2,6)-linked sialic acid receptors typically found in the upper respiratory tract of humans) the overall conclusion is the same: these pathogenic H7N9 viruses can readily replicate in mammalian respiratory tract cells and can readily transmit through direct contact and, to a lesser extent, through airway droplets. Indeed, as these paper were published, Dr. Yuelong Shu, director of the Chinese National Influenza Center at the China CDC in Beijing, was reported as acknowledging that “Contrary to previously published reports, the deadly H7N9 bird flu can spread from person to person and may be a serious threat to humans…”
Solid data on possible asymptomatic transmission of the virus will have to await until the virus returns this fall, if it does.
 H7N9 Update - Death Toll Mounts to 43 in 133 Total Cases
H7N9 Update - Death Toll Mounts to 43 in 133 Total Cases
06Jul13
The WHO is reporting that the total number of lab-confirmed cases of H7N9 globally has increased to 133. This represents the addition of a single case since the last update and this single case is the 15M patient from Jiangsu Province who was found to be co-infected with seasonal H3N2 and H7N9 after being hospitalized on April 26th. The patient recovered quickly and was discharged from hospital on May 2nd. The details of this case are close to those described in a recent article in The Lancet (see the note, below, on H7N9 from 15Jun13).
Sadly, the WHO report also notes that death toll in China has risen to 43, up from 39 just a few weeks ago. The 4 additional cases should include the fatality (56M) from Shanghai reported in the Chinese press last week. Sadly, that case (#47) is the husband of case #14 who died earlier. Case #47 had been hospitalized since April 11th.
With less than a dozen patients remaining in hospital, it is clear the case fatality rate (CFR) for H7N9 in this outbreak will settle near 35%. this is lower than the CFR of another avian influenza/A virus, H5N1 (at 59%), but substantially higher than the CFR associated with the 2009-2010 swine flu pandemic (around 1%). Thus, a news report earlier this week stating that "H7N9 is most adapted bird flu for human-to-human transmission..." is worrisome since the virus may have a lower barrier to becoming a true human pandemic virus.
 2009 H1N1p Still Deadly Across the Globe
2009 H1N1p Still Deadly Across the Globe
06Jul13
The 2009 H1N1p virus continues to ply its deadly trade in South Asia, Southeast Asia, and South America. An outbreak of H1N1p in northern Chile has reportedly left 11 dead. Notably, the regional rate of infection (at 148 patients per 100,000 population) is more than six times higher than in the rest of the country. This news follows reports last month of outbreaks of 2009 H1N1p in Argentina, Columbia, and especially Venezuela (see item below from June 16th).
In India, the western state of Maharashtra has already reported 84 deaths from H1N1p in the first six months of the year, on track to beat last year's fatality count of 135. According to the Times of India article, "...experts fear that more Mumbaikars may fall victim as hundreds from the city travel every day to Pune and Nashik...". And in Vietnam, the 11th death from H1N1p has been reported this year, up from 3 in mid-June.
The differential geographic populations of influenza/A remain a matter of great interest. The factors which mitigate the composition of local circulating influenza/A strains remain enigmatic. However, it is clear that the 2009 H1N1p remains a pandemic virus "in play" and hence worthy of continued close scrutiny.
 Human Infections with Swine Flu Variant H3N2v Increase
Human Infections with Swine Flu Variant H3N2v Increase
05Jul13
The variant swine influenza, H3N2v, is back, as noted by Recombinomics (see here and here). The first 4 cases of human infection were confirmed in attendees from a fair in Grant County, Indiana, at the end of June. Two of the four cases had reported contact with pigs. Then, on July 4th, another 8 lab-confirmed cases were identified in nearby Hancock County, Indiana. Again, all lab-confirmed cases had attended a county fair but in the latter cases, most had contact with pigs. It should be noted that 29 swine also tested positive for the virus between the two fairs. Sequences from 3/4 of the initial cases from Grant County have been obtained and released. As noted in the latter report from Recombinomics, all three sequences "matched human 2012 H3N2v cases and all three sequences were closely related to each other, signaling clonal expansion." Recombinomics also notes that this year the H3N2v virus has appeared about a month earlier than last year, potentially signalling a robust season for the virus.
As a result of these new infections, the CDC issued, today, an official Health Advisory updating "H3N2v case definitions and recommendations for H3N2v surveillance for the summer and fall of 2013."
 CDC Reviews Past Seasonal Flu Season
CDC Reviews Past Seasonal Flu Season
14Jun13
In this week’s Morbidity and Mortality Weekly Report (MMWR), the CDC has reviewed the 2012-2013 seasonal flu season (September 30, 2012–May 18, 2013) in the US. The document contains two major sections, data and editorial, both interesting. The past season is characterized as “moderately severe” and, as is typical of influenza, possesses attributes different than the “historical norm” or expectation. Attributes that stand out include:
1. The season started early and peaked early (both due to H3N2 activity) but managed to persist to standard lengths due to a (typical) late season surge of influenza B.
2. The pediatric influenza mortality was the highest ever recorded for a seasonal flu season. A total of 149 laboratory-confirmed, influenza-associated pediatric deaths were reported with 40 of the deaths occurring in just 3 states (Texas, New York, and Florida). Influenza-associated pediatric mortality only became a nationally-notifiable condition in 2004 and since that time the annual number of influenza-associated pediatric deaths has ranged between 34-123, excluding the roughly 18 month period of the 2009 H1N1 pandemic period where 348 pediatric fatalities were recorded. Influenza B infection accounted for 53% of all pediatric influenza-associated fatalities even though influenza B accounted for only 36% of viral samples characterized over the season.
3. The percentage of deaths attributed to pneumonia and influenza (P&I) exceeded the epidemic threshold for 13 consecutive weeks (over weeks 1-13 in 2013), reaching a peak of 9.9% during week 3. This peak value is higher than any observed since 2008. Similarly, the peak percentage of outpatient visits for influenza-like illness (ILI) was 6.1% and occurred at week 52 of 2012. This peak value greatly exceeds that for the preceding season (at 2.4%) and is one of the highest ever observed since ILI surveillance commenced in 1997 (it was 7.7% in the 2009 pandemic outbreak). This peak value is even above the peak values observed in two recent years where A/H3N2 also dominated in circulation: the 2007–08 (at 6.0%) and 2010–11 (at 4.6%) influenza seasons. In both of the latter seasons, peak values in ILI were observed in February.
4. The past influenza season was particularly hard on the elderly. “The number and rate of influenza-associated hospitalizations among adults aged ≥65 years during the 2012–13 influenza season are the highest since systematic data collection on laboratory-confirmed, influenza-associated hospitalization in adults began in the 2005–06 season. Hospitalization rates for those aged ≥65 years were 191 per 100,000 population, two and a half times the highest rate previously reported for this age group.”
The A/H3N2 viruses that struck the US this past season clearly made a surprisingly notable mark and the prevalence of the A/H3N2 virus is in contrast to the dominance of A/H1N1 last year (2011-2012 season). Geographical segregation is still at play. In 2011-2012, A/H2N2 was the predominant circulating virus in Canada but not here and the 2009 H1N1p virus continues to dominate in select regions, including much of South and Central America. No one knows for sure what portends for the 2013-2014 season in the US, but the sudden, dramatic appearance of A/H7N9 in China, a spike of A/H5N1 in parts of SE Asia, and a possibly resurgent A/H1N1p in India constitute an ominous and potent mix for concern. As noted by the CDC review, “Testing for seasonal influenza viruses and monitoring for novel influenza A virus infections should continue year-round, as should specimen submission to CDC for further antigenic and genetic analysis and antiviral resistance monitoring.”
 MERS Update – More Deaths & Another Country
MERS Update – More Deaths & Another Country
12Jul13
The first patient (82M) to be diagnosed and treated within the United Arab Emirates for MERS-CoV was reported by CIDRAP yesterday, citing local sources. This brings the global total of confirmed cases to 82 with 45 fatalities.
The WHO issued another GAR on 09Jul13 in which it notes an apparent change in the type of confirmed cases reported since its last GAR. Half of the recently reported cases are asymptomatic and are occurring in women and young children, a marked shift from earlier demographics. It has also updated its current view of MERS-CoV transmission. “The recent mild and asymptomatic cases raise concerns about the possibility of large numbers of milder cases going undetected. While it is clear that human-to-human transmission does occur, it is not clear whether transmission is sustained in the community. The currently observed pattern of disease occurrence could be consistent either with ongoing transmission in an animal reservoir with sporadic spillover into humans resulting in non-sustained clusters, or unrecognized sustained transmission among humans with occasional severe cases.”
Hats off to Recombinomics who have long been arguing that unrecognized sustained transmission among humans is a distinct possibility (see here).
 MERS-CoV Confirmed Cases Hits 90 with 45 Deaths
MERS-CoV Confirmed Cases Hits 90 with 45 Deaths
21Jul13
The SARS-like corona virus, MERS-CoV, continues to rack up the number of lab-confirmed cases and fatalities. Last Thursday, the WHO issued another Global Alert & Response update that noted "Globally, from September 2012 to date, WHO has been informed of a total of 88 laboratory-confirmed cases of infection with MERS-CoV, including 45 deaths." The bulk of the GAR idescribes six cases recently reported to the WHO: 2 from The Kingdom of Saudi Arabia [KSA] and 4 from The United Arab Emirates [UAE]. For the latter, "...the four cases are health care workers from two hospitals in Abu Dhabi who took care of an earlier laboratory-confirmed patient. Of these, two cases, a 28-year-old man and 30-year-old woman, did not develop symptoms of illness. The other two cases, both women of 30 and 40 years old, had mild upper respiratory symptoms and are in stable condition."
For the cases in KSA, both "...have mild symptoms and are not hospitalized. They are from Asir region. The first case is a 26-year-old man who is a close contact with a previously laboratory-confirmed case and the second case is a 42-year-old woman who is a health care worker."
On Friday, the CDC listed on its webpage a total of 90 cases with 45 fatalities. Details on the additional two cases were provided in an update today from the WHO. "WHO has been informed of two additional laboratory-confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in Saudi Arabia. Both the cases are currently critically ill and hospitalized in ICUs. The first case is a 41-year-old Saudi male in Riyadh who presented to the hospital with symptoms on 15 July. The second patient is a 59-year-old Saudi female in the Al-Ahsa governorate. She presented with symptoms on 11 July. Both patients have underlying medical conditions, but neither patient has had contact with known MERS-CoV confirmed cases or animals. "
Of particular note is the additional descriptions of mild symptoms or cases that were asymptomatic. As laid out by Recombinomics, the existence of mild and/or asymptomatic cases is "indicating MERS-CoV was transmitting in sustained manner by the milder cases not linked to severe hospitalized index cases. There is no ongoing surveillance for these milder cases." This could prove to be a crucial deficit in controlling viral spread.
 H7N9: This Week's Developments
H7N9: This Week's Developments
28May13 Updated 29May13
The number of confirmed cases of H7N9 influenza in China was holding steady at 130 (with one additional case in Taiwan; now discharged from hospital) as recently as yesterday, marking an abrupt end to this wave of H7N9 in China, as no new cases of human infection have been reported since early May. That changed today with the Xinhua News agency reporting a new confirmed case of human infection in Beijing. The global count of confirmed cases of H7N9 infection now stands at 132 with 37 deaths and 76 patients having recovered and been discharged from hospital. The CFR for H7N9 is settling in around 30%.
The new case in Beijing (6M) "developed symptoms including fever and headache on May 21 and he was sent to a hospital for medical treatment on the same day. His body temperature returned to normal on May 23 and he returned to kindergarten the next day..." according to the Xinhua News agency report. He was subsequently found to be positive for H7N9. This is not the first case of mild or even asymptomatic H7N9 infection in young children and highlights the ability of the virus to operate in "stealth" mode as it propagates, unseen, through the (pediatric) population.
The geographic spread of the virus remains a concern not just in humans, but also in relevant zoonotic reservoirs, such as poultry and pigs. Last week, an international team of investigators reported in Science Express that ferrets could transmit the virus by direct contact and, to a lesser degree, via airborne droplets. Ferrets are often used in viral transmission studies to estimate human-to-human spread. The investigators also found that pigs can indeed be infected by H7N9 but do not appear to transmit the virus. In this light, the confirmation last week of H7N9 in a poultry isolate from Guangdong Province marks the spread of the virus ever closer to another high-density urban population.
It is also interesting to note that China's Ministry of Agriculture has now nearly completed a massive sweep of avian and poultry environments for H7N9. Of nearly 900,000 samples taken, a mere 53 tested positive for H7N9. Of these 53, "Fifty-one positive samples were from 18 live poultry markets in Shanghai, Anhui, Zhejiang, Jiangsu, Henan, Shandong, Guangdong, Jiangxi and Fujian, the MOA said in a statement. The other two positive samples were from wild pigeons in Nanjing, capital of Jiangsu Province and domestic pigeons in Nantong, in Jiangsu Province." These observations underscore the need to identify the source of human infection and what is happening in widely geodistributed live-poultry markets that is absent from wild birds and poultry farms.
Finally, another potential source of great concern was illuminated in a new report that appeared online yesterday in The Lancet from a team of investigators in China and entitled "Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance." In this study, the investigators followed 14 patients admitted to the Shanghai Public Health Clinical Centre in April of 2013. All of the patients presented with pneumonia and seven of these came to require mechanical ventilation. Three of these patients subsequently required ECMO and 2 of these three patients subsequently died. All of patients were treated with neuraminidase inhibitors (oseltamivir and peramivir) but those patients on ECMO maintained high viral loads despite oseltamivir and peramivir therapy. Indeed, 2/3 ECMO patient rapidly developed resistance to neuraminidase inhibitors. One of the patients showed dominance of the resistant strain by 9 days after treatment began. The relative ease and rapidity for the onset of neuraminidase inhibitor resistance is worrisome. Oseltamivir (Tamiflu) is the backbone of available antiviral therapies and has been heavily stockpiled by governments around the world for pandemic preparedness. If the utility of these drugs were obviated by the virus, especially for a virus that provokes only weak immune responses in early vaccine efforts, no effective medical interventions would remain.
It is widely believed that influenza will die down in China over the summer months before potentially returning again this fall. In anticipation of a possible return, continued surveillance, study, and preparation remain the order of the day.
 Case Count for MERS-CoV (hCoV-EMC) Nears 50
Case Count for MERS-CoV (hCoV-EMC) Nears 50
29May13
Five new cases of confirmed infection with the novel SARS-like virus, hCoV-EMC (now MERS-CoV), were reported today, all in the Kingdom of Saudi Arabia (KSA). The five case are from Eastern KSA, "but not from Al-Ahsa, where an outbreak began in a health care facility in April 2013. The patients had underlying medical conditions which required multiple hospital visits." Three of the five confirmed cases have died. In addition, France's first MERS-CoV patient has died, as has a previously-reported patient from the Al-Ahsa region of KSA.
These cases bring the global count to 49 confirmed cases since September of last year with 27 fatalities. For a complete listing of all cases, see Sharon Sander's comprehensive table at FluTrackers.com.
Also, a detail clinical look at the two MERS-CoV patients in France was published today in The Lancet. A major conclusion from this paper is that for the second patient, a French native with no travel to the Middle East, but who shared a hospital room with the first patient for 3 days, "the incubation period was estimated at 9–12 days for the second case. No secondary transmission was documented in hospital staff despite the absence of specific protective measures before the diagnosis of MERS-CoV was suspected." This a a longer incubation period than previously thought and may suggest that longer quarantine periods are in order to prevent spreading to contacts.
Speaking yesterday at the 66th World Health Assembly in Geneva, Dr. Margaret Chan, Director-General of the WHO, stated:
"Looking at the overall world health situation, my greatest concern right now is the novel coronavirus [MERS-CoV].
We understand too little about this virus when viewed against the magnitude of its potential threat.
Any new disease that is emerging faster than our understanding is never under control.
We do not know where the virus hides in nature. We do not know how people are getting infected. Until we answer these question, we are empty-handed when it comes to prevention.
These are alarm bells. And we must respond."
 The Tide of Seasonal Influenza Slips Away in N. America
The Tide of Seasonal Influenza Slips Away in N. America
17May13
The latest set of influenza data (see the data here; for the week ending May 11th; Week 19) released by the CDC today again shows a continued decay in most flu-associated parameters. The % of respiratory specimens tested as positive for influenza ticked up slightly to 5.1% [down from 6.5% two weeks ago and up from 4.1% last week] while the % of doctors' visits for ILI remained at 0.9% [from 1.0% two weeks ago and 0.9% last week], well below the national baseline of 2.2%. Altogether, 1 state reported low flu activity while 49 states and NYC experienced only minimal activity. A/H3N2 virus accounts for 55.4% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 34.8% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 9.8%
More recently, influenza B has accounted for over half (75.8% versus 67.2% last week) of typed viruses for week 19 while all influenza A viruses accounted for only 24.2% (versus 32.8% last week).
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index bumped up a bit to 6.4% (compared to 7.0% last week and 6.6% in the prior week). The epidemic threshold for the P&I index for Week 19 is 7.1%.
The number of total influenza-associated pediatric deaths for the season increased to 139 with 1 new fatality reported for Week 19. The one death was associated with an influenza A virus for which the subtype was not determined. The cumulative pediatric death toll for this season makes the 2012-2013 season one of the worst in years.
Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased slightly to 44.2/100,000, up from 44.2/100,000 the week prior. As of the end of Week 19, 12,348 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 191/100,000. The vast majority (>79%) of all influenza- associated hospitalizations were due to influenza A infection
The season influenza season terminated as of the data up to 30Apr13. We will continue to update the seasonal flu data (see here) as released by the CDC.
 H1N1p Flu Outbreak in Tibet - One Pediatric Fatality
H1N1p Flu Outbreak in Tibet - One Pediatric Fatality
16May13
An outbreak of influenza, initially reported as H1N1 but later (and apparently mistakenly) as H5N1, infected 65 children in the Guangxi Autonomous Region of Tibet last week. One child has died and 5 other children have been hospitalized in critical condition. The source of the infection has not been established, but reportedly infected chickens brought in from Nanning and sold at cut-rate prices. It was also reported yesterday that Tibet is wrestling with an avian outbreak of H5N1. As noted in the initial report, 3 other confirmed pediatric cases of H1N1p occurred in early April at a school about 180 km away from the present outbreak. H1N1p has been a recent problem in other South Asian countries. For example, Vietnam has recently reported on an outbreak of H1N1p in one of its northern provinces, an outbreak at a boarding school where 3 children had tested positive for the virus.
 Seasonal Influenza: At Last, an Abatement in Pediatric Deaths, Too!
Seasonal Influenza: At Last, an Abatement in Pediatric Deaths, Too!
11May13
The latest set of influenza data (see the data here; for the week ending May 3rd; Week 18) released by the CDC yesterday again shows a continued decay in most flu-associated parameters. The % of respiratory specimens tested as positive for influenza dropped sharply to 4.1% [down from 7.4% two weeks ago and 6.5% last week] while the % of doctors' visits for ILI dropped to 0.9% [from 1.1% two weeks ago and 1.0% last week], well below the national baseline of 2.2%. Altogether, 49 states and NYC experienced only minimal activity with one state, SD, not reporting. A/H3N2 virus accounts for 55.4% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 34.6% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 9.9%
More recently, influenza B has accounted for over half (67.2% versus 66.7% last week) of typed viruses for week 18 while all influenza A viruses accounted for only 32.8% (versus 33.3% last week).
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index bumped up a bit to 7.0% (compared to 6.6% last week and 6.7% in the prior week). The epidemic threshold for the P&I index for Week 18 is 7.2%.
The number of total influenza-associated pediatric deaths for the season increased to 138 with 1 new fatality reported for Week 18. The one death was associated with an influenza A virus for which the subtype was not determined. This marks a dramatic reduction in pediatric deaths as compared to the preceding weeks and is welcome news. The cumulative pediatric death toll for this season makes the 2012-2013 season one of the worst in years.
Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations remained at 44.2/100,000, as it was the week prior. As of the end of Week 18, 12,330 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 190/100,000. The vast majority (>79%) of all influenza- associated hospitalizations were due to influenza A infection
The season influenza season terminates as of the data up to 30Apr13. We will continue to update the seasonal flu data (see here) as released by the CDC.
 Another H7N9 Fatality; Toll Now at 33
Another H7N9 Fatality; Toll Now at 33
11May13
Another human H7N9 fatality has been reported out of Shanghai in China. The victim (83F; Case # 37) was originally hospitalized in stable condition after first experiencing symptoms on the 7th of April. Once the initial site of the H7N9 outbreak, Shanghai has but 4 confirmed cases remaining in hospital while 14 have died and 15 have recovered and been discharged.
 5 More Cases of MERS-CoV (hCoV-EMC); 1st French Cases
5 More Cases of MERS-CoV (hCoV-EMC); 1st French Cases
09May13
Five new cases of confirmed infection with the novel SARS-like virus, hCoV-EMC (now MERS-CoV), have been reported: two today in the Kingdom of Saudi Arabia [KSA], and three in France.
As detailed in an email to ProMED by the Deputy Minister for Public Health for the Kingdom of Saudi Arabia, the case specifics, identified retrospectively, are as follows:
Case 14: 48M with multiple comorbidities. Start of symptoms 29 Apr 2013 and confirmed by lab testing. He is in stable condition in hospital.
Case 15: 58M with comorbidity. Start of symptoms 6 Apr 2013. His repeat testing was positive and he fully recovered and was discharged on 3 May 2013.
One should note that Case 15 has an onset date of April 6th, well before the other cases that have been reported this month from the KSA. This significantly extends the time frame that the MERS-CoV was circulating in humans in this region of the KSA. also of interest is that all of the patients in the KSA this month have become ill in hospital, including two family members who were visiting a relative.
Yesterday, the WHO reported that the first case of MERS-CoV has been reported in France. The 65M patient had recently returned to Douai, France from Dubai and fell ill on 23Apr13. He is currently in the ICU on a respirator. Late today, it was announced that two individuals who have been in contact with the 65M patient have now fallen ill: a 50+M patient in the same ward as the 65M patient and the attending 35M doctor. Both of the latter came in contact with the 65M patient when he was hospitalized in the town of Valenciennes. Both of the latter patients are now themselves in single rooms in separate hospitals.
Since the MERS-CoV virus emerged in September of 2012, 31 confirmed cases of human infection have occurred with 18 of the cases fatal. The existence of clusters of cases in the UK, KSA, and now France clearly shows at least limited human-to-human transmission. As reported today by Helen Branswell, the KSA is bringing in outside experts to deal with outbreak in al Hofuf, including a key expert from Toronto on SARS, Dr. Allison McGeer. But as noted in the same article, the biggest break for investigators may be the 65M patient in France. He traveled to UAE as part of a package tour and these tours are often tightly orchestrated. This may allow investigators to hone in on a source of infection which is currently unknown (as it is for H7N9).
 Human H7N9 Cases Now 130 with 31 Fatalities
Human H7N9 Cases Now 130 with 31 Fatalities
07May13
The number of confirmed cases of H7N9 influenza in China has increased to 128 with the announcements (see WebLink) of 2 additional confirmed cases in Fujian Province, increasing the total number of confirmed cases in China to 129. There is also a previously reported confirmed case in Taiwan. One of the two news cases (9M) has already recovered and been discharged from hospital. Four additional fatalities were announced but no other details were provided other than that 2 of the fatalities were in Jiangsu Province, 1 was in Zhejiang Province, and another was in Anhui Province. Our previous description of a recent fatal case (55M) in Hunan province has now been reassigned to a previously reported Jiangxi patient (who was in fact a resident of Hunan province but was being treated in the former province). A total of 5 H7N9 patients were discharged from the hospital since last Friday lifting the total number of recovered patients to 42.
The weekly reporting scheme for new cases, previously announced by the Chinese government, is due for announcement tomorrow. This new information could indicate whether the peak of cases has already occurred in China (or at least in some provinces/municipalities) or whether the lull has been due to the shift to a weekly report. Of note, the SE Chinese province of Guangdong has been added to the list of affected regions after H7N9 was found in an agricultural sample from a poultry market. This continues last week's trend of increasing geographical spread for the H7N9 virus.
A full list of the 129 confirmed human cases of H7N9 infection is tabulated at this web page.
In other matters of note, the Director of the CDC, Dr. Thomas Frieden, told Reuters, in an article carried by the Huffington Post, that "...the current strain of bird flu that is causing illness and deaths in China cannot spark a pandemic in its current form - but he added that there is no guarantee it will not mutate and cause a serious pandemic." This perspective was confirmed at the end of last week by one of Europe's leading experts, Dr Angus Nicoll. In article published online on Saturday by the Singapore paper Today, Dr. Nicoll is paraphrased as stating that "Human cases of a deadly new strain of bird flu that has killed 27 people in China are likely to crop up in Europe and around the world but that should not cause undue alarm.." Thus, identifying the source of H7N9 infections remains a major priority (perhaps the major priority) for the infectious disease community.
 Human H7N9 Cases Now 129 with 27 Fatalities
Human H7N9 Cases Now 129 with 27 Fatalities
03May13
The number of confirmed cases of H7N9 influenza in China has increased to 128 with the announcements (see here) of 1 additional, fatal case in Hunan province. Two additional fatalities in cases previously reported from Jiangsu province were also announced but no other details were provided. The most recent case (55M) is Hunan province's third confirmed case and first fatality. A total of 10 H7N9 patients were discharged from the hospital today, including a 38M (Case #49) who is reportedly the first patient with severe symptoms to recover. He was in hospital a total of 22 days.
The weekly reporting scheme previously announced by the Chinese government is now clearly in effect and details about specific cases are already becoming scarcer.
A full list of the 129 confirmed human cases of H7N9 infection is tabulated at this web page.
 Seasonal Influenza: Even More Abatement
Seasonal Influenza: Even More Abatement
03May13
The latest set of influenza data (see the data here; for the week ending Apr. 27th; Week 17) released by the CDC today again shows a continued decay in most flu-associated parameters, with one notable exception (pediatric influenza mortality, a lagging indicator), while influenza B retains it predominance of any residual flu activity. The % of respiratory specimens tested as positive for influenza dropped to 6.5% [down from 9.3% two weeks ago and 7.4% last week] while the % of doctors' visits for ILI dropped to 1.0% [from 1.3% two weeks ago and 1.1% last week], well below the national baseline of 2.2%. Altogether, only 1 state experienced low flu activity. Fully 48 states and NYC experienced only minimal activity. A/H3N2 virus accounts for 54.7% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 35.2% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 10.1%
As in the past 12 weeks, influenza B accounted for over half (66.7% versus 64.8% last week) of typed viruses for week 17 while all influenza A viruses accounted for only 33.3% (versus 35.2% last week). Inspection of the stacked column chart (here) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past five reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index dropped a bit to at 6.6% (compared to 6.7% last week and 7.2% in the prior week). The epidemic threshold for the P&I index for Week 16 is 7.2%.
However, the number of total influenza-associated pediatric deaths for the season increased to 137 with 7 new fatalities reported for Week 17. One death was associated with an influenza A virus for which the subtype was not determined, one death was associated with A/H3 influenza, and five deaths were associated with influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 44.2/100,000, up from 43.9/100,000 the week prior. As of the end of Week 17, 12,314 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 190/100,000. The vast majority (>79%) of all influenza- associated hospitalizations were due to influenza A infection
The season influenza season should continue to ebb over the coming weeks as even influenza B exits the scene.
 Seasonal Influenza: Abatement Continues
Seasonal Influenza: Abatement Continues
26Apr13
The latest set of influenza data (see the data here; for the week ending Apr. 20th; Week 16) released by the CDC today again shows a continued decay in most flu-associated parameters, with one notable exception (pediatric influenza mortality, a lagging indicator), while influenza B retains it predominance of any residual flu activity. The % of respiratory specimens tested as positive for influenza dropped to 7.4% [down from 10.9% two weeks ago and 9.3% last week] while the % of doctors' visits for ILI dropped to 1.1% [from 1.5% two weeks ago and 1.3% last week], well below the national baseline of 2.2%. Altogether, only 1 state experienced low flu activity. Fully 49 states and NYC experienced only minimal activity. A/H3N2 virus accounts for 57.2% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 33.2% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 9.5%
As in the past 11 weeks, influenza B accounted for over half (64.8% versus 73.7% last week) of typed viruses for week 16 while all influenza A viruses accounted for only 35.2% (versus 26.3% last week). Inspection of the stacked column chart (here) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past four reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index remained at 6.7% (compared to 7.2% last week and 7.2% in the prior week). The epidemic threshold for the P&I index for Week 16 is 7.3%.
However, the number of total influenza-associated pediatric deaths for the season increased to 131 with 5 new fatalities reported for Week 16. One death was associated with an influenza A virus for which the subtype was not determined and four deaths were associated with influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 43.9/100,000, up from 43.7/100,000 the week prior. As of the end of Week 16, 12,250 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 190/100,000. The vast majority (>79%) of all influenza- associated hospitalizations were due to influenza A infection
The season influenza season should continue to ebb over the coming weeks as even influenza B exits the scene.
 Human H7N9 Cases in China Now 109 with 22 Fatalities as Flu Spreads Further
Human H7N9 Cases in China Now 109 with 22 Fatalities as Flu Spreads Further
24Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 108 with the announcement of 3 additional cases in Zhejiang (2) and Anhui provinces. The previously reported suspected case in Shandong province has also now been confirmed, bringing the total cases in China to 108. No additional cases or fatalities were reported today in China, but the first report of a confirmed case of H7N9 in Taiwan was announced.
The Taiwanese patient (53M) returned from a trip to Jiangsu province on April 9th and came down with his first symptoms on April 12th. He is currently hospitalized in critical condition. This case is notable for three other reasons besides being the first confirmed case in Taiwan:
1) The patient tested negative for H7N9 twice previously (by throat swab specimens) while hospitalized, underscoring the problems with identifying H7N9 as the causative agent. It was a third analysis (this time of a of a sputum sample) that led to identification of H7N9 by RT-PCR.
2) It is standard practice to monitor close contacts of infected patients for signs of H7N9. In this case, three health care workers (HCWs) tending the patient are now showing symptoms of H7N9 infection and are being monitored. What is interesting about this point is that the three HCWs were wearing full protective gear while tending the patient while three other HCWs, who did not wear protective gear, have not shown any symptoms of infection, at least not yet.
3) Among other prior medical conditions, the patient is a carrier of hepatitis B. Given the difficulties in identifying a source of infection so far and the lack of compelling evidence of sustained human-to-human transmission, this observation raises the intriguing possibility that severe cases of H7N9 infection in humans require co-infection by other, heretofore unidentified, viruses.
One additional fatality, from previously reported cases, was also reported in Zhejiang province. The fatality (86M; case #81) fell ill on Apr. 13th.
A full list of the 109 confirmed human cases of H7N9 infection is tabulated at this web page. The significance of the current "pause" in new infections in China remains to be determined.
 Human H7N9 Cases in China Now 105 with 21 Fatalities as Flu Expands to New Province
Human H7N9 Cases in China Now 105 with 21 Fatalities as Flu Expands to New Province
22Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 105 with the announcements (see here, here, and here) of 9 additional cases in Shanghai, Jiangsu, and Zhejiang provinces and, for the first time, in Shandong province. Three additional fatalities, from previously reported cases, were also reported in Shanghai and Zhejiang provinces, though details on the Shanghai fatality are currently limited. One of the deaths (62F; case #53) fell ill on Mar. 29nd while the other (76M; case # 99) fell ill on April 8th. The other fatality (in Shanghai) is likely Case #78, but confirmation is still outstanding. Several instances of patient recovery were also reported. The Shandong patient tested positive for H7N9 by PCR is awaiting final confirmation by the China CDC.
A full list of the 105 confirmed human cases of H7N9 infection is tabulated at this web page.
 First Human H5N1 Fatality in Bangladesh
First Human H5N1 Fatality in Bangladesh
20Apr13
The WHO has confirmed the recent death of a 23 month-old boy from Bangladesh as that region's first human fatality due to H5N1 infection. The case is unusual in that the patient experienced none of the typical symptoms associated with H5N1 infections.
Since the first H5N1 case was identified in Bangladesh in May of 2008, there have been a total of 7 human cases. The child in this case was in close proximity to poultry. Currently, four influenza viruses are circulating in Bangladesh: H1N1p, H5N1, H3N2 and H9N2.
Earlier this month, the first human H5N1 fatality in Vietnam in over a year was reported and Cambodia has experienced 10 cases just this year according to the WHO.
As noted by ProMED, "As of 12 Mar 2013 globally there have been 622 human cases of avian A/(H5N1) influenza virus infection, resulting in 371 deaths in 15 countries." Since September of 2012, there have been a total of 16 cases of H5N1 infection in humans, mainly in SE Asia and Egypt, resulting in 12 deaths.
 Seasonal Influenza Continues to Abate - Jump in Ped. Morbidity
Seasonal Influenza Continues to Abate - Jump in Ped. Morbidity
19Apr13
The latest set of influenza data (see the data here; for the week ending Apr. 13th; Week 15) released by the CDC today shows a continued “down tick” in most flu-associated parameters, with one notable exception, while influenza B retains it predominance of residual flu activity. The % of respiratory specimens tested as positive for influenza dropped to 9.3% [down from 11.3% two weeks ago and 10.9% last week] while the % of doctors' visits for ILI dropped to 1.3% [from 1.8% two weeks ago and 1.5% last week], well below the national baseline of 2.2%. Altogether, 1 state experienced moderate activity and another low flu activity. Fully 48 states and NYC experienced only minimal activity. A/H3N2 virus accounts for 56% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 34.3% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 9.7%.
As in the past 10 weeks, influenza B accounted for over half (73.7%) of typed viruses for week 15 while all influenza A viruses accounted for only 26.3%. Inspection of the stacked column chart (here) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past four reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index remained at 7.2% (compared to 7.2% last week and 7.4% in the prior week). The epidemic threshold for the P&I index for Week 15 is 7.4%.
However, the number of total influenza-associated pediatric deaths for the season increased to 126 with 10 new fatalities reported for Week 15. One death was associated with 2009 H1N1 virus, one death was associated with an influenza A virus for which the subtype was not determined, and one death was associated with A/H3N2 influenza virus. Seven deaths were associated with influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 43.7/100,000, up from 43.2/100,000 the week prior. As of the end of Week 14, 12,170 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 188/100,000. The vast majority (>79%) of all influenza- associated hospitalizations were due to influenza A infection.
The season influenza season should continue to ebb over the coming weeks as even influenza B exits the scene.
 Human H7N9 Cases in China Now 60 with 13 Fatalities as Flu Expands to New Provinces
Human H7N9 Cases in China Now 60 with 13 Fatalities as Flu Expands to New Provinces
14Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 60 with the announcement of 11 additional cases in Shanghai, Jiangsu, and Zhejiang provinces and, for the first time, in Henan province and Beijing. Two additional fatalities, from previously reported cases, were also announced in Shanghai. One of the deaths (67F; case #12) fell ill on Mar. 22nd while the other (77M; case # 26) fell ill on April 3rd. Case 26 is of note because the last information on this patient listed his condition as "stable".
A full list of the 60 confirmed human cases of H7N9 infection is tabulated at on this web page.
The expansion of H7N9 cases outside of the initial set (of Shanghai, Zhejiang, Jiangsu, and Anhui) may be another important milestone in this evolving story. The range of reported human infections now spans may more miles and deepens, with the absence of H7N9 in Beijing bird populations so far, the mystery of how humans are being infected.
The reader is also directed to two outstanding publications in the New England Journal of Medicine on H7N9 and its pandemic potential. The articles can be found here and here.
 Human H7N9 Cases in China Increases to 28 with 9 Fatalities
Human H7N9 Cases in China Increases to 28 with 9 Fatalities
09Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 28 with the announcement of four additional cases (62M, 77M, 79M, & 51F) in Shanghai and Zhejiang provinces and two additional fatalities. Both of the Shanghai patients and one of the Zhejiang patients are in stable condition while the remaining Zhejiang patient is in critical condition. One of the deaths (83M) was the 6th listed case of confirmed H7N9 infection while the other (35M) was the third. A full list of the 28 human cases of H7N9 infection is tabulated at the left.
In related news, the CDC has activated its Emergency Operations Center (EOC) in Atlanta yesterday to support the response to the H7N9 influenza outbreak in China, according to a report by CIDRAP. "The EOC was activated at level 2, the second of three levels. Level 1, the highest, signals an agency-wide response."
 H1N1p Found in Elephant Seals Off California Coast
H1N1p Found in Elephant Seals Off California Coast
16May13
An team of scientists from the US and from Chile have made a startling observation. The scientists were performing research to understand zoonotic transfer of influenza among species, an effort they started in 2007. Starting early in 2009, the investigators took to obtaining some 900 nasal swabs from northern elephant seals and nine other species of marine mammal living off the coast of central California. While influenza virus are known to infect seals, it was nonetheless a big surprise when 30 seals showed ongoing or prior exposure to the 2009 H1N1p virus. This is the first report of H1N1p in a marine mammal.
According to one of the investigators, "The seals on land in early 2010 tested negative before they went to sea, but when they returned from sea in spring 2010, they tested positive. So the question is where did it come from?” The seals had satellite tags, so the investigators at least knew where the seals had been in the intervening months when they picked up the virus. The answer: the Northeast Pacific.
The study was published yesterday in PLoS ONE. The study "provides evidence for cross species transmission of influenza viruses in free-ranging wildlife and movement of influenza viruses between humans and wildlife." And it sheds yet another light on the complex nature of interspecies transmission dynamics for influenza.
 More H7N9 Fatalities; Toll Now at 36
More H7N9 Fatalities; Toll Now at 36
15May13
Another three human H7N9 fatalities has been reported from China in the last two days, bringing the death toll to 36. Yesterday, the death toll was announced at 35 but no details were provided. Today, another death was reported from Hunan Province: a 64F (Case #120) who at one time was reportedly improving. 5 additional patients have been discharged from hospital in the last two days: Case #124 and 4 unspecified patients from Jiangsu Province (see here and here).
There has been a virtual dearth of new cases reported over the last week or so. This might reflect a sudden disappearance of H7N9 due to seasonal factors or it could reflect the effectiveness of control measures in the poultry population. As the CFR settles in the mid-30 percent region, one can only await the virus' next move, if any.
 Case Count for MERS-CoV (hCoV-EMC) Tops 40
Case Count for MERS-CoV (hCoV-EMC) Tops 40
15May13
A fist full of new cases of confirmed infection with the novel SARS-like virus, hCoV-EMC (now MERS-CoV), have been reported over the past week with 41 confirmed cases since September of last year, 22 of them since mid-April in the Kingdom of Saudi Arabia (KSA). 9 of these 22 cases have been fatal. For a complete listing of all cases, see Sharon Sander's comprehensive table at FluTrackers.com. It also appears that more cases may emanate from France as lab confirmation in several cases is pending. The WHO also provided an update today at their Global alert and Response page.
Unfolding events in KSA appear to indicate that at least limited community transmission of the virus is underway (see this story from CIDRAP).
 Human H7N9 Cases Now 131 with 32 Fatalities
Human H7N9 Cases Now 131 with 32 Fatalities
09May13
The number of confirmed cases of H7N9 influenza in China has increased to 130 with the announcements (see here) of 1 additional confirmed case (79F) in Jiangxi Province. One additional fatality from a previously reported case in Henan province was also announced. This most recent death (56M) is the province's first fatal case, the other three provincial patients having previously been discharged from hospital. Another patient was discharged from the hospital yesterday, a 80M (Case #123) from Jiangxi Province.
A full list of the 131 confirmed human cases of H7N9 infection is tabulated at this web page.
There have now been two consecutive days with no newly confirmed cases of human infection by H7N9 in China, marking a dramatic fall from the rapidity with which the first 100 or so cases came in. This may be due to the extensive efforts of the Chinese government in closing poultry markets and culling birds. Let's hope so. Influenza is a particularly tricky beast, so a couple of events to continue to watch:
1. A new scientific report just out shows that the number of flu infections in pigs is increasing in south China (see this report from the The Standard (Hong Kong) for a description). The pig is an excellent zoonotic mixing chamber for influenza and a source of previous influenzas that impact humans. Given the mammalian adaptation features of not only H7N9, but also H5N1 (active in SE Asia) and H1N1p (active in Vietnam and South Asia), a geographically focused cauldron of viral reassortment is possible over the coming months. Each virus has specific strengths and weaknesses as a candidate pandemic strain, and their ability to gain additional pandemic characteristics is greatly facilitated by this geographical cauldron.
2. While it is unknown whether H7N9 will ever be a pandemic strain, it is worth remembering that the WHO has called H7N9 an espcially dangerous virus for humans, once infected. As such, there is plenty of activity focused on generating a vaccines to H7N9. But in yesterday's New Scientist, in an article describing the prudent measures of the CDC/FDA to prepare for a H7N9 epidemic or pandemic [including already invoking "Emergency Use Authorization" for H7N9 diagnostic kits], a potentially significant problem is reported: the H7N9 virus elicits only a mild immune response in humans. In fact, the human immune response to the virus is so weak that "Virologists at the European Flu Summit in Brussels last week told New Scientist that early results show 13 times more H7N9 virus is needed to elicit a protective immune response than is needed for ordinary flu." That means more antigen per vaccine dose and less doses produced per unit time. Unfortunately, this is consistent with earlier statements by the folks at EpiVax (see remarks in 16Apr13 entry below) who predicted that H7N9 would be a "stealth virus" to the human immune system since it presented so few T-cell epitopes on its HA surface. They concluded that " "... it will be difficult to make effective vaccines and low cost diagnostics for the newly emerging virus."
3. This spring outbreak of H7N9 is perhaps a heraldic or pre-heraldic wave as has been put forward for the 1918 Spanish flu outbreak in the U.S. (see, for example, this article). This might position the current H7N9 virus as a "precursor" strain" that could circulate for up to several years prior to a pandemic outbreak. In this case, the unique age-distribution of confirmed cases would parallel the excess mortality observed in the elderly during the 1915-16 season, as described in the cited article. Thus, keeping a close eye for a "age signature shift" would seem prudent.
Finally, an online news article from the BBC reports on a scientific study just published in JAMA Psychiatry that shows that "Flu during pregnancy may increase the risk of the unborn child developing bipolar disorder later in life...". This result echoes prior studies where influenza infection during pregnancy was associated with a higher risk of schizophrenia (see this article). It should be noted that the risks reported in these studies are relative and the absolute risk remains small.
 3 More Cases in Outbreak of Novel Human β2c Coronavirus (hCoV-EMC)
3 More Cases in Outbreak of Novel Human β2c Coronavirus (hCoV-EMC)
07May13
Three new cases of confirmed infection with the novel SARS-like virus, hCoV-EMC, have been reported in the Kingdom of Saudi Arabia [KSA], two of them fatal.
As detailed in an email to ProMED by the Deputy Minister for Public Health for the Kingdom of Saudi Arabia, the case specifics are as follows:
Case 11: 62F with multiple comorbidities. Start of symptoms [19 Apr 2013] and deceased [3 May 2013]
Case 12: 71M with multiple comorbidities. Start of symptoms [15 Apr 2013], deceased [3 May 2013]
Case 13: 58F with comorbidities. Start of symptoms [1 May 2013] and currently ventilated in critical but stable condition.
The Deputy Minister goes on to say that "..there is no apparent community transmission and transmission seem linked to one HCF [health care facility]."
An article appearing today on-line at the Wall Street Journal proffers that "Saudi Arabia's announcements in the past five days of seven new deaths from a SARS-like virus have heightened fears that the Mideast outbreak is entering a more-aggressive phase."
The specifics surrounding the underlying co-morbidities for these three newest patients (as well as the prior 10 reported this month) could provide insights into the significance of this outbreak. To date, 22 of the 30 confirmed cases that have occurred globally have been reported in the Kingdom of Saudi Arabia. Thirteen of the cases reported from KSA have occurred this month and so far 7/13 cases have been fatal.
On a positive note, Michael Katze (Univ. of Washington) and colleagues have just published a lovely paper on the differences in host response (at the level of the transcriptome) between SARS virus and hCoV-EMC. At 12 hours post infection, "HCoV-EMC induced a massive dysregulation of the host transcriptome, to a much greater extent than SARS-CoV. Both viruses induced a similar activation of pattern recognition receptors and the interleukin 17 (IL-17) pathway, but HCoV-EMC specifically down-regulated the expression of several genes within the antigen presentation pathway, including both type I and II major histocompatibility complex (MHC) genes." In addition, they identified potential drug candidates specifically targeting hCoV-EMC elicited proteins, thus defining a rapid path in response to newly emergent pathogens.
 Another H5N1 Fatality
Another H5N1 Fatality
06May13
Another human H5N1 fatality has been reported, this time out of Egypt. The victim (25F) was originally hospitalized on the 29th of April complaining of fever and shortness of breath. The patient expired before lab results confirmed the presence of H5N1 influenza.
According to the latest (26Apr13) update on H5N1 from the WHO, "...
6 new laboratory-confirmed human cases with influenza A(H5N1) virus infection were reported to WHO from Bangladesh (1), Cambodia (1), Egypt (2) and Viet Nam (2). The investigations into these concluded that they were sporadic cases and that the appearance of sporadic cases is expected and will likely occur in the future."
Certainly the mixing pot in SE Asia of H7N9, H1N1p, and H5N1 creates an added dimension of concern given the potential for novel reassortants arising that pick up pandemic characteristics.
 Outbreak of Novel Human β2c Coronavirus (hCoV-EMC) Reported in Saudi Arabia
Outbreak of Novel Human β2c Coronavirus (hCoV-EMC) Reported in Saudi Arabia
03May13 Updated 04May13
The news out of Saudi Arabia yesterday was stunning. Seven more patients were reportedly confirmed as infected with the novel human corona virus hCoV-EMC and five of these patients had died. Three more confirmed infections were announced on May 4th. Nine of the ten new confirmed cases are male and may involve one or more family clusters. All of the patients had underlying co-morbidities. Besides the five deaths in this group, three other patients are in critical condition and two are hospitalized but doing well. The global incidence of confirmed human infections by this SARS-like virus has now climbed to 27 with 16 fatalities.
As detailed in an email to ProMED by the Deputy Minister for Public Health for the Kingdom of Saudi Arabia, the case specifics are as follows:
Case 1: 59M. Date of onset of symptoms [14 Apr 2013] and passed away [19 Apr 2013].
Case2: 24M. Date of symptoms [17 Apr 2013] and still in ICU in critical but stable condition.
Case 3: 87M. Date of symptoms [17 Apr 2013] and passed away [28 Apr 2013].
Case 4: 58M. Date of symptoms [22 Apr 2013] still in ICU in stable but critical condition.
Case 5: 94M. Date of symptoms [22 Apr 2013] and passed away [26 Apr 2013].
Case 6: 56M. Date of Symptoms [22 Apr 2013] and passed away [30 Apr 2013].
Case 7: 56M. Date of symptoms [22 Apr 2013] and passed away [29 Apr 2013].
Case 8: 53F. Date of symptoms [27 Apr 2013] she is in stable but critical condition.
Case 9: 50M. Date of symptoms [30 Apr 2013] with pneumonia and he is well on the inpatient ward.
Case 10: 33M. Family contact of a deceased patient. Date of symptoms [28 Apr 2013]. Inpatient in the medical ward and doing well.
The specifics surrounding the underlying co-morbidities for all of these patients could provide insights into the significance of this outbreak. To date, 19 of the 27 confirmed cases have occurred in the Kingdom of Saudi Arabia.
 Human H7N9 Cases Now 128 with 24 Fatalities; Is H7N9 on Holiday?
Human H7N9 Cases Now 128 with 24 Fatalities; Is H7N9 on Holiday?
01May13
The number of confirmed cases of H7N9 influenza in China has increased to 127 with the announcements (see here and here) of 2 additional cases: one more Fujian and another in Hunan province. No additional fatalities have been reported in the past two days. Indeed, there has not been a new case of H7N9 reported in Shanghai for 10 days, perhaps due to aggressive closing of poultry markets and extensive culling. Thus, while the virus has greatly expanded its geographical reach over the past week or so, the number of new confirmed cases has plummeted. As noted today in an editorial in The Boston Globe, "China’s annual “Golden Week” holiday, which started Monday, is a time for millions of Chinese to vacation in neighboring countries, boosting commercial activity and person-to-person contact." The next few weeks will no doubt prove interesting.
A full list of the 128 confirmed human cases of H7N9 infection is tabulated at this web page.
Also of note, a new paper out today in The Lancet explores the origin and reassortment events that gave rise to pathogenic H7N9. The authors found that H7N9 virus might have evolved from at least four different avian influenza strains and that the current H7N9 virus behind the ongoing outbreak can likely be divided into two subclades. Specifically, the authors conclude that "The HA and NA genes might originate from duck avian influenza viruses, which might have obtained the viral genes from migratory birds a year previously, whereas the internal genes might come from chicken avian influenza viruses. We believe that the estimated times to most recent common ancestor for the eight genomic fragments and the frequent poultry transportation in China account for the increased number of confirmed sporadic cases of human infection."
Finally, Dr. David Fisman (University of Toronto) has submitted a most interesting note on ProMED concerning the unusual age & gender characteristics exhibited by H7N9 patients in China. Dr. Fisman writes that "while concerning, application of basic epidemiology suggests that the current picture of H7N9 influenza in China is subject to case ascertainment bias, which is likely contributing to marked inflation of the apparent CFR. The age and gender distribution of cases relative to the population is reminiscent of that seen in legionellosis, an environmentally abundant pathogen that appears to preferentially cause recognized infection in older males." A corollary to this line of reasoning is that there are many more subclinical cases of human H7N9 infection than currently thought, especially among the young. Indeed, "the true risk of infection in younger people could be approximated by the apparent risk of infection in older individuals" which would raise the total number of infections to ~500 but would substantially reduce the apparent CFR. A widespread ecological distribution of the avian H7N9 could explain the low incidence of detection in various poultry populations.
 Human H7N9 Cases Now 126 with 24 Fatalities as Flu Expands to New Province
Human H7N9 Cases Now 126 with 24 Fatalities as Flu Expands to New Province
29Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 125 with the announcements (see here, here, and here) of 7 additional cases in Shandong, Jiangxi, Fujian, and Zhejiang provinces as well as, for the first time, in Hunan province. One additional fatality was also reported in Shanghai and one additional recovery was reported in Henan province. The fatality (89M; case #78) fell ill on April 12 and was initially reported to be in stable condition. The patient apparently succumbed after his condition worsened and a 12 day course of treatment failed. The reported patient recovery (38M) was initially reported to be in critical condition but was discharged from hospital yesterday. The new confirmed case from Shandong province (4M) is the son of the province's first confirmed case (Case #103) and represents another "microcluster" of likely human-to-human transmission. With the previously reported confirmed case in Taiwan, the global count of confirmed cases now stands at 128. 79 patients remain hospitalized, many of them in serious or critical condition.
A full list of the 126 confirmed human cases of H7N9 infection is tabulated at this web page.
 H7N9 Spreads Further Afoot: 119 Confirmed Cases, 23 Fatalities, and 2 New Provinces
H7N9 Spreads Further Afoot: 119 Confirmed Cases, 23 Fatalities, and 2 New Provinces
26Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 118 with the announcements [link1, link2, link3, link4, link5] of 10 additional cases in Zhejiang (3), Jiangsu (3) and Henan (1) provinces, as well as 3 cases appearing in Jiangxi (2) and Fujian (1) provinces for the first time. The previously announced case of H7N9 in Taiwan brings the global total of confirmed human H7N9 cases to 119. Thus, this week has seen a notable spread of confirmed cases to three new Chinese provinces (Shandong, Jiangxi, and Fujian) and to Taiwan.
One additional fatality, previously reported in Jiangsu province on April 24th but without details, was further specified. The fatality (32F; case #7) fell ill on Mar. 21st. The total number of fatalities due to H7N9 infection now stands at 23.
A full list of the 119 confirmed human cases of H7N9 infection is tabulated at this web page. The significance of the current "pause" in new infections in Shanghai may be due to aggressive closing of poultry markets and culling or to the new government policy of updating cases weekly (every Wednesday) or both.
A set of important papers have been published in the last day or two and the reader is encouraged to review them:
1. A study published in The Lancet that shows that avian isolates obtained at local markets in China (and thus epidemiologically related to initial human isolates from 4 patients (two of whom died) with known poultry contact) can contain H7N9 viruses with genomes very similar to those in patients. From a small sampling of 20 chickens, 57 ducks, 4 quail, and 5 pigeons, H7N9 was detected in 40% of pigeons and 20% of chickens while none of the sampled ducks or quail had the virus. From genomic sequencing of a chicken isolate, “All viral gene segments were of avian origin. The H7 of the isolated viruses was closest to that of the H7N3 virus from domestic ducks in Zhejiang, whereas the N9 was closest to that of the wild bird H7N9 virus in South Korea. We noted Gln226Leu and Gly186Val substitutions in human virus H7 (associated with increased affinity for α-2,6-linked sialic acid receptors) and the PB2 Asp701Asn mutation (associated with mammalian adaptation). Ser31Asn mutation, which is associated with adamantane resistance, was noted in viral M2.” However, important sequence signatures of mammalian adaptation were absent from the poultry isolates though present in clinical isolates (see also this link), specifically the Q226L mutation in HA and the D701N or E627K mutation in PB2. The authors state that these mutations could be acquired upon infection of the patient but it is also possible that another intermediate mammalian species harbors the virus first, prior to human infection. Also of interest was the authors’ observation that “Sputum specimens were more likely to test positive for the H7N9 virus than were samples from throat swabs.” This may have import for surveillance efforts since it is much more difficult to obtain deep lung samples (sputum) that nasopharyngeal swabs.
2. A preliminary report, published in the New England Journal of Medicine, describes initial epidemiological analysis of the H7N9 outbreak in China using the first 82 confirmed patients. The major conclusion of the report is that “Most persons with confirmed H7N9 virus infection were critically ill and epidemiologically unrelated. Laboratory-confirmed human-to-human H7N9 virus transmission was not documented among close contacts, but such transmission could not be ruled out in two families.”
Finally, the reader is referred to two new columns in Nature, both free. The first is an column by Peter Horby that makes the case for why we should keep a critical eye on H7N9 despite having skepticism about a possible global pandemic. And the second is a column by Declan Butler on mapping the H7N9 outbreak and how it is useful in monitoring potential pandemic pathogens.
 Third 2009 H1N1p Flu Fatality in Vietnam This Month
Third 2009 H1N1p Flu Fatality in Vietnam This Month
24Apr13
A news report out of Vietnam describes the third fatality this month from 2009 H1N1p influenza infection. The victim (12F) came down with the flu after a visit from her brother-in-law who was infected with the virus. Two other family members also became ill but recovered.
Earlier this month, two other fatalities (23M and 40M) were reported as succumbing to 2009 H1N1p infection. the news article above cites the vice chief of Vietnam's National Institute of Hygiene and Epidemiology as stating that the 2009 H1N1 type A influenza virus accounts for nearly half of the flu cases detected this year.
These reports sound similar to the situation in India these past few months where the severity of the disease (acute respiratory distress) in a younger population of patients echoes "pandemic virus"-like characteristics much more than a mere seasonal flu-like strain. Detailed sequencing of the viral genome from patient isolates is clearly warranted.
 Confirmed H7N9 Cases in China Increase to 96 With 18 Fatalities
Confirmed H7N9 Cases in China Increase to 96 With 18 Fatalities
20Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 96 with the announcement of 19 additional cases in Anhui, Jiangsu, and Zhejiang provinces. An additional two fatalities, one in Jiangsu province, were announced over the past two days. As of today's total of 96 confirmed cases, the distribution by province is: 1 in Beijing, 33 in Shanghai, 3 in the central province of Henan, 33 in the eastern province of Zhejiang, 23 in the eastern province of Jiangsu and 3 in Anhui Province.
A full list of the 96 confirmed human cases of H7N9 infection is tabulated on this web page. The two new fatalities are Case #61 and Case #87. The latter case is of note due to the short time between the case being reported and the announcement of death. In the last two days, three patients have been discharged (out of a total of 7): Cases #18,21, and 27. Sixty seven of the 96 patients remain hospitalized.
Recombinomics has described a new H7N9 sequences (A/Zhejiang/DTID-ZJU01/2013) deposited from an April 3 collection from a male patient in Zhejiang Province. The HA gene sequence is identical to that of a prior human isolate: A/Anhui/1/2013. However, unlike the four prior human sequences, "... the Zhejiang PB2 sequence does not have E627K. However, the PB2 sequence does have D701N, which also enhances transmisison in mammals, as seen in H5N1 transmission experiments." Thus, all five isolates from humans have PB2 sequences possess mammalian adaptation changes that distinguish them from avian H7N9 sequences currently in circulation in China.
Other lines of evidence underscore nagging questions about the source of infection for humans by H7N9. An article in Forbes, citing the state-run newspaper, Shanghai Daily, states that "More than half of the victims have had no contact with poultry, the newspaper said, citing agencies and its own reporting." Along another line, an article in the New York Times, citing China’s state-run news agency, Xinhua, noted that "China’s agricultural authorities were insisting the H7N9 virus was still confined to live poultry markets. The news agency said that 47,801 samples had been collected from 1,000 poultry markets, habitats and farms from across China, and that agricultural authorities said that 39 tested positive for H7N9. " 39 positives out of almost 48,000 avian samples is a very low prevalence and similar testing in pigs has also come up negative.
Another perplexing attribute of the human H7N9 virus is found in the characteristics of the confirmed patients. Many more males than females are reported as confirmed cases and, until fairly recently, the age distribution among patients is skewed towards patients over 55. Both of these attributes are at odds with "typical" pandemic viruses as evidenced by the recent behavior of the 2009 H1N1p virus as well as human infections by H5N1. The observed skewing in the age distribution of H7N9-infected patients is more typical of bad seasona influenza. However, the age distribution in confirmed patients may be changing, skewing towards the younger patients typically infected by pandemic viruses where there is no pre-existing immune memory to help ward off the pathogen. Keep an eye on the age demographic in confirmed patients over the next few weeks. A shift towards higher pathogenicity in younger patients would signal acquisition of additional "pandemic virus"-like characterstics for the human H7N9 virus.
 Human H7N9 Cases in China Increase to 77 With 16 Fatalities
Human H7N9 Cases in China Increase to 77 With 16 Fatalities
16Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 77 with the announcement of 17 additional cases in Anhui, Jiangsu, and Zhejiang provinces and a later story, citing the China CDC, announcing six additional cases in Shanghai province. Of particular note is that 5/6 Shanghai cases are reported as retrospective diagnoses. An additional three fatalities, one in Jiangsu province, were announced Monday (with two of three fatalities only mentioned in the late-breaking story). As of today's total of 77 confirmed cases, there is one in Beijing, 30 in Shanghai, two in the central province of Henan, 21 in the eastern province of Zhejiang, 20 in the eastern province of Jiangsu and three in Anhui Province. With these additions, the case count for H7N9 has now outpaced that for global H5N1 infections last year (see this Commentary).
A full list of the 77 confirmed human cases of H7N9 infection is tabulated on this web page. The one known new fatality (out of three today) is Case #45.
There were also expressions of extreme concern today (see weblink1 & weblink2) over the announcement yesterday of a 4M in Beijing who is asymptomatic for H7N9 despite testing positive for the virus. The 4M is a neighbor of Case #44, a 7F from Beijing who is scheduled for release from the hospital tomorrow, having fully recovered. The concern is that there may be a large number of asymptomatic patients and that we're only focused on the subset of patients who are most ill and hence directly tested for the H7N9 virus. Such a large number of aysmptomatic patients would be possible if there was sustained human-to-human [H2H] transmission. Almost all official reports state that there is no evidence of sustained H2H. In the case of sustained H2H with large numbers of asymptomatic patients, the recently observed geographical expansion of confirmed cases away from the Eastern coast of China into Beijing and Henan province is very worrisome. The concept of sustained H2H transmission through largely asymptomatic patients is bolstered by the genomic sequencing of clinical isolates of H7N9, as first noted by Recombinomics. These clinical isolates contain mammalian adaptation mutations, some of which are not seen in isolates of H7N9 from recent poultry specimens.
In other events today, the CDC has updated their "Interim Guidance for Infection Control Within Healthcare Settings When Caring for Patients with Confirmed, Probable, or Cases Under Investigation of Avian Influenza A(H7N9) Virus Infection". The WHO announced that "An international team of flu experts will go to China this week to help with investigations into the deadly H7N9 virus..." Finally, a team at EpiVax is predicting that human H7N9 is a "stealth virus" largely unseen by the human immune system (due to a very low number of T cell epitopes) and that "... it will be difficult to make effective vaccines and low cost diagnostics for the newly emerging virus (also called H7N9/A/Shanghai/1/2013)." They conclude that the H7N9 virus has "...serious potential for rapid expansion on a global scale."
 Human H7N9 Cases in China Jumps to 43 with 11 Fatalities
Human H7N9 Cases in China Jumps to 43 with 11 Fatalities
12Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 43 with the announcement of 15 additional cases in Shanghai, Jiangsu, and Zhejiang provinces and two additional fatalities. One of the deaths (74M; case #17)) fell ill on Mar. 28th while the other (74M; case # 36) fell ill on Mar. 31st. Both fatalities were from Shanghai. A full list of the 43 human cases of H7N9 infection is tabulated at the left.
In related news, the CDC has announced today that, based on previous experience with H5N1,"...it’s likely that some limited human-to-human spread of this H7N9 virus will be detected." In the same announcement, the CDC reported that "On Thursday April 11, CDC received the first H7N9 virus isolate from China..." and this isolate will be used to support standard pandemic preparedness, including vaccine generation. Yesterday, the CDC updated its interim guidance for infection control involving possible H7N9 infections.
In their H7N9 update published yesterday, WHO noted that "If the current pattern of sporadic infections continues, WHO will cease frequent reporting of case numbers, and focus its Disease Outbreak News on new developments or changes in the pattern or presentation of infections."
 Seasonal Influenza Continues to Fade Out in U.S.
Seasonal Influenza Continues to Fade Out in U.S.
12Apr13
The latest set of influenza data (see the data here; for the week ending Apr. 7th; Week 14) released by the CDC today shows a continued “down tick” in most flu-associated parameters, even below threshold levels, while influenza B expands it predominance of residual flu activity. The % of respiratory specimens tested as positive for influenza dropped to 10.9% [down from 13.2% two weeks ago and 11.3% last week] while the % of doctors' visits for ILI remained at 1.5% [from 1.8% the past two weeks], and well below the national baseline of 2.2%. Altogether, only 2 states experienced low ILI activity. Fully 48 states and NYC experienced only minimal ILI activity. A/H3N2 virus accounts for 57.2% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 32.8% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 10%.
As in the past 9 weeks, influenza B accounted for over half (71%) of typed viruses for week 14 while all influenza A viruses accounted for only 28.9%. Inspection of the stacked column chart (here) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past three reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index has now dropped to 7.2% (compared to 7.4% last week and 7.5% in the prior week). The epidemic threshold for the P&I index for Week 14 is 7.4%.
However, the number of total influenza-associated pediatric deaths for the season increased to 116 with 5 new fatalities reported for Week 14. One death was associated with an A/H3 influenza virus while four deaths were associated with influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 43.2/100,000, up from 42.3/100,000 the week prior. As of the end of Week 14, 12,052 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 184/100,000. The vast majority (>81%) of all influenza- associated hospitalizations were due to influenza A infection.
The season influenza season should continue to ebb over the coming weeks as even influenza B leaves the scene.
 Human H7N9 Cases in China Increases to 24 with 7 Fatalities
Human H7N9 Cases in China Increases to 24 with 7 Fatalities
08Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 24 with the announcement of two additional cases (85M & 25F) in Jiangsu and an additional fatal case (64M) in Shangai. For the fatal case, the diagnosis of H7N9 infection was arrived at posthumously. Both of the Jiangsu patients are in critical condition. A full list of the 24 human cases of H7N9 infection is tabulated at the left.
In related news, another report today from the South China Morning Post noted that "There is no proof that the H7N9 bird flu virus is being transmitted between people in China, the World Health Organisation said on Monday, despite several members of a family falling ill in Shanghai." And still another story notes that the 4 yr old Shanghai boy hospitalized with H7N9 has now "basically recovered".
 Human H7N9 Infections in China Expand to 21 with 6 Fatalities
Human H7N9 Infections in China Expand to 21 with 6 Fatalities
05Apr13 Updated: 06Apr13 & 07Apr13
The number of confirmed cases of H7N9 influenza in China has increased to 16 with six fatalities according to the WHO in an update released today. The table (left) summarizes the 16 cases to date. Also of note, more than 520 close contacts of the confirmed cases are being closely monitored. An investigation is currently ongoing in Jiangsu province of a contact that has developed disease symptoms. WHO officials have been quoted as saying that that there was no sign of 'sustained human-to-human transmission' of the H7N9 virus in China. On April 6th, a Canadian news source has reported the number of confirmed cases has climbed to 18.
In related events, Chinese authorities have closed three public markets in Shanghai, banned poultry imports from elsewhere in the country, and culled over 20,000 poultry in the city in an effort to curb the virus [link]. Culling has also been reported in a second Chinese city (Hangzhou; 100 miles SW of Shanghai) after quail were identified bearing H7N9.
In a curious note, a report out of China describes a lake near Shanghai suddenly filled with dead fish. This follows an analogous set of reports [mid-March; link]citing the sudden deaths of more than 6,000 pigs, recovered in rivers near Shanghai and dumped there by nearby breeding facilities. The cited report also quotes several months where 6-7000 pigs were dying per month, though their deaths were largely attributed to porcine circovirus (due, in part, to the absence of any known swine zoonoses). But as noted by Recombinomics, pigs could provide a secondary or intermediate zoonotic reservoir for the virus, but one that could facilitate mammalian adaptation.
In the U.S., the CDC has issued a health advisory to physicians to help identify H7N9 infections, though no cases have been found anywhere in the U.S. [link]. The CDC has developed a diagnostic test to evaluate ill travelers returning from China. The CDC is also “…developing diagnostic test kits that it will distribute to China and other countries to ensure rapid diagnosis of this strain of flu.” The CDC is also already working with vaccine manufactures to develop an H7N9 vaccine just in case.
An avian influenza strain, newly capable of infecting humans while already displaying molecular features of mammalian adaptation and resulting in severe disease in humans but not in birds, warrants careful, wary scrutiny. To this end, public health officials from around the world are beginning “to lay out their concerns” [link] as we wait for the virus to show us its next card.
 Influenza Season Draws to a Close
Influenza Season Draws to a Close
30Mar13
The latest set of influenza data (see figures at left; for the week ending Mar. 23rd; Week 12) released by the CDC today shows a continued shift in influenza cases from influenza type A viral infections towards type B and a pronounced “down tick” in most flu-associated parameters, even below threshold levels. The % of respiratory specimens tested as positive for influenza dropped to 13.2% [down from 14.3% two weeks ago and 16.3% last week] while the % of doctors' visits for ILI decreased to 1.8% [from 2.6% two weeks ago and 2.2% last week], below the national baseline of 2.2%. Altogether, only 1 state [ ] experienced moderate flu activity while 3 states and NYC experienced low ILI activity. Fully 46 states experienced only minimal ILI activity. A/H3N2 virus accounts for 58% of all antigenically characterized viruses characterized since Oct. 1, 2012 while influenza B accounts for 32.6% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 9.4%.
As in the past 6 weeks, influenza B accounted for over half (73.5%) of typed viruses for week 12 while all influenza A viruses accounted for only 26.5%. Inspection of the stacked column chart (left) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past two reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index remained at 7.5% (compared to 7.6% last week and 7.6% in the prior week). The epidemic threshold for the P&I index for Week 12 is 7.5%.
The number of total influenza-associated pediatric deaths for the season increased to 110 with 5 new fatalities reported for Week 12. One of the deaths was associated with A/H3N2 infection, two were associated with influenza A viruses for which the subtype was not determined, and the other two deaths were due to infection by influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 41.8/100,000, up from 40.5/100,000 the week prior. As of the end of Week 12, 11,639 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 51% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 180/100,000. The vast majority (>82%) of all influenza- associated hospitalizations were due to influenza A infection.
The season influenza season should continue to ebb over the coming weeks as even influenza B leaves the scene.
 Still More Worries Around Influenza 2009 H1N1p
Still More Worries Around Influenza 2009 H1N1p
20Mar13
Earlier this week, the BBC reported that Australian scientists have found that a significant fraction of the influenza 2009 H1N1p virus now in global circulation is resistant to Tamiflu (oseltamivir), a major anti-viral drug that has been massively stockpiled by governments across the globe. This could suggest that the pandemic virus is following the path of its seasonal H1N1 cousin in becoming Tamiflu resistant virtually everywhere in the globe, effectively rendering the drug useless against that virus. In particular, the scientists have observed Tamiflu-resistant virus in people outside of a hospital setting and who have never taken the drug. Presently, the resistant virus is found in about 2% of clinical isolates globally. Though still a small percentage, this level may be sufficient to catalyze rapid propagation around the world. The Australian scientists report that the virus they have studied in circulation is still sensitive to Relenza (zanamivir), another anti-influenza A drug.
 Influenza B Sinks Its Teeth
Influenza B Sinks Its Teeth
15Mar13
The latest set of new data (see figures at left; for the week ending Mar. 9th; Week 10) released by the CDC today indicates a continued shifting of influenza from largely type A towards type B and a slight “uptick” in some flu-associated parameters. For example, the number of states reporting moderate levels of flu activity was up slightly over last week’s report from 4 to 5 states. However, the % of respiratory specimens tested as positive for influenza dropped to 14.3% [down from 16.9% two weeks ago and 17.2% last week] while the % of doctors' visits for ILI increased to 2.6% [from 2.7% two weeks ago and 2.3% last week], above the national baseline of 2.2%. Altogether, 5 states [MD, MS, NJ, TX, and VA ] and New York City experienced moderate flu activity while 12 states experienced low ILI activity. A/H3N2 virus accounts for 62.6% of all antigenically characterized viruses characterized since Oct. 1, 2012 while influenza B accounts for 28.7% of all isolates. Isolates antigenically characterized as 2009 H1N1p remained at 8.7%.
However, for the fourth week in a row, influenza B accounted for over half (64.4%) of typed viruses for week 10 while all influenza A viruses accounted for only 35.6% [about the same %’s as last week]. Inspection of the stacked column chart (left) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more constant. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season. Depending upon the persistence of influenza B in the coming weeks, the U.S. could be expected to linger near the epidemic thresholds, as noted last week.
Other (mainly lagging) indicators of flu activity remained elevated. Most notably, the pneumonia and influenza (P & I) mortality index decreased to 7.6% (down from 7.7% last week and 8.4% in the prior week). The epidemic threshold for the P&I index for Week 10 is 7.5%. However as we noted last week, the cyclical seasonal baseline is near its apex (at week 10) and a persistence of influenza B over the coming weeks may keep the P&I index at or near the epidemic threshold.
The number of total influenza-associated pediatric deaths for the season increased to 99 with 12 new fatalities reported for Week 10. One of the deaths was associated with A/H3N2 infection, two were associated with influenza A where sub-typing was not performed, and nine deaths were due to infection by influenza B. TX has been particularly hard hit with a total of 14 pediatric deaths this season. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 39.6/100,000, up from 38.5/100,000 the week prior. As of the end of Week 10, 11,043 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for more than 51% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 170/100,000. The vast majority (>83%) of all influenza- associated hospitalizations were due to influenza A infection.
 CDC Issues Alerts Over Deadly, Novel Corona Virus [N-CoV]
CDC Issues Alerts Over Deadly, Novel Corona Virus [N-CoV]
08Mar13
The CDC today issued a Health Advisory Notice to health care providers, giving guidance for the evaluation of severe respiratory illness associated with a novel coronavirus. This follows the publication yesterday in Morbidity and Mortality Weekly Report of an update to the public health community in the U.S. concerning the emergent novel corona virus (N-CoV , a.k.a. London1_novel CoV 2012) that has already claimed 8 lives since September of last year, the most recent just last month. The WHO has issued a Global Alert & Response (GAR) on this same coronavirus in December of 2012.
The CDC states in their note that they will continue to “….work closely with the World Health Organization (WHO) and other partners to better understand the public health risk posed by a novel coronavirus...” and have provided updated guidance on their website. The CDC update was motivated by new developments including a recent cluster that provides the first clear evidence of human-to-human transmission of the N-CoV, coinfection of N-CoV with another pathogen (influenza A), and a case of mild illness associated with N-CoV infection.
While there have been no reports of infection in the U.S., a total of 14 people (in Saudi Arabia, Qatar, Jordan, and the United Kingdom) have been confirmed as having an infection caused by the novel coronavirus. The virus is a distant relative of the SARS CoV that emerged in 2002-4, causing severe acute respiratory infections, flu-like symptoms (fever, chills, headache, and myalgia), lymphopenia, and potentially ARDS. All told, the SARS virus resulted in roughly 8000 cases worldwide with an overall fatality rate of 10%.
The new guidance from the CDC on N-CoV states:
“Persons who develop severe acute lower respiratory illness within 10 days after traveling from the Arabian Peninsula or neighboring countries* should continue to be evaluated according to current guidelines. In particular, persons who meet the following criteria for “patient under investigation” (PUI) should be reported to state and local health departments and evaluated for novel coronavirus infection:
• A person with an acute respiratory infection, which may include fever (≥ 38°C , 100.4°F) and cough; AND
• suspicion of pulmonary parenchymal disease (e.g., pneumonia or acute respiratory distress syndrome based on clinical or radiological evidence of consolidation); AND
• history of travel from the Arabian Peninsula or neighboring countries* within 10 days; AND
• not already explained by any other infection or etiology, including all clinically indicated tests for community-acquired pneumonia† according to local management guidelines.
CDC requests that state and local health departments report PUIs for novel coronavirus to CDC.”
The N-CoV commands careful monitoring since it results in symptomology similar to SARS and has already been shown to be well-adapted to infect human cells: it easily penetrate the passageways of the lung, easily grows on human epithelial cells, and can evade the innate immune system as readily as a cold virus. It is often and repeatedly stated that the N-CoV virus is most closely related to a corona virus found in bats but, as pointed out by Recombinomics, there are significant differences in the nucleotide sequences between N-CoV and bat viruses. Finally, there is likely a bias in the tracking of persons infected with N-CoV towards only the most severe cases, as evidenced by the high case fatality rate (>50%), and the low level of the virus in the upper respiratory tract which could lead to false negatives in standard testing. All of this strongly suggests human-to-human transmission of N-CoV without the benefit of a direct zoonotic intermediary.
If N-CoV behaves as SARS did a decade ago, the CDC Health Advisory Notice will be viewed as timely and we can expect more human cases in the near term.
 Rare Superbugs Here and Abroad
Rare Superbugs Here and Abroad
06Mar13
This week’s early release version of the CDC’s Morbidity and Mortality Weekly Report highlights the rise in carbapenem-resistant Enterobacteriaceae in U.S. health-care facilities. The Enterobacteriaceae are a large family of gram-negative bacilli that are normal inhabitants of the gastrointestinal tract of mammals, including humans. These pathogens are a common cause of community-acquired and health-care–acquired infections. In particular, the health-care–associated Enterobacteriaceae most commonly reported to the CDC are Escherichia coli, Klebsiella , and Enterobacter species.
The past several decades have seen the spread of Enterobacteriaceae with resistance to broad-spectrum antimicrobials. Physicians in the U.S. have used carbapenem antibiotics (e.g. imipenem, meropenem, doripenem, and ertapenem) to treat infections caused by resistant organisms. There isn't much left in the quiver after carbapenems.
Carbapenem-resistant Enterobacteriaceae (CRE) were relatively uncommon in the U.S. before 2000. The latest data from the CDC now shows that the proportion of Enterobacteriaceae that were CRE increased from 1.2% in 2001 to 4.2% in 2011 and to 4.6% in 2012. While antibiotic resistance in CREs can be complex and resistance factors are easily exchanged with other bacteria, a common mechanism of resistance is the bacterial production of enzymes that can inactivate carbapenems, such as carbapenemases. Two well-known examples of carbapenemases are KPC (Klebsiella pneumoniae carbapenemase) and NDM (New Delhi metallo-beta-lactamase).
The issue of CREs is important since such infections, though still low in incidence, can have associated mortality rates of 40-50%. According to a report in the Washington Post, Thomas Frieden, director of the Centers for Disease Control and Prevention, said at a news conference: “It’s not often that our scientists come to me and say we have a very serious problem and we need to sound an alarm. But that’s exactly what we are doing today.” The CDC recommends a six-step "detect and protect" program for healthcare providers aimed at stemming the spread of CRE.
Meanwhile, officials at the UK Health Protection Agency (HPA) have noted a staggering 25% increase in the number of cases of gonorrhea over the past year in England. This increase is occurring as drug-resistant strains of pathogens causing sexually transmitted infections (STIs) spread globally. According to the CDC, the number of cases In the US alone is estimated at about 700,000 a year. According to a report on Medscape News, itself citing a Reuters story, "...effective treatment with antibiotics has been compromised by growing resistance, the HPA said, noting "a drift towards decreased susceptibility" of gonorrhea infections to the cephalosporins that are normally recommended as treatment".
Finally, a news report out of the University of Rochester spotlights a potential weakness of at least one superbug, drug-resistant E. coli. Drs. Gloria Culver and Keith Connolly have focused their research on bacterial ribosomes, an essential cellular component for viability. Specifically, they found that a balance is necessary between two bacterial proteins, RbfA and KsgA, for ribosomes to assemble and carry out their mission in protein biosynthesis. Disrupting the balance between these two proteins could disrupt bacterial protein synthesis and therefore would constitute a novel mechanism of antibiotic action.
 Influenza Takes a Breather
Influenza Takes a Breather
in U.S.
01Mar13
The latest set of new data (see figures at left; for the week ending Feb. 23rd; Week 8) released by the CDC today indicates a continued ebbing of influenza from peak levels at the end of last year with moderate-to-high levels of activity remaining in just 12 states. The % of influenza-positive tests of respiratory specimens clocked in at 16.9% [down from 19.7% two weeks ago and 16.8% last week] and the % of doctors' visits for ILI decreased slightly to 2.7% [from 3.2% two weeks ago and 2.8% last week] [though still above the national baseline of 2.2%]. Altogether, 12 states and New York City experienced moderate ILI activity while another 15 states reported low activity. A/H3N2 virus accounts for 62.7% of all antigenically characterized viruses while influenza B accounts for 30% of all isolates characterized since Oct. 1, 2012. Isolates antigenically characterized as 2009 H1N1p fell to 7.3%.
Other (mainly lagging) indicators of flu activity remained elevated. Most notably, the pneumonia and influenza (P & I) mortality index decreased to 8.4% (down from 8.6% last week and 9.1% in the prior week). The epidemic threshold for the P&I index for Week 8 is 7.5% The number of influenza associated pediatric deaths increased to 81 with 3 new fatalities reported last week. One of the deaths was associated with H3N2 infection, one was associated with influenza A where subtyping was not performed, and one deaths was due to infection by influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of flu hospitalizations increased again to 36.7/100,000, up from 34.2/100,000 the week prior. As of the end of Week 8, 10,227 laboratory-confirmed influenza-associated hospitalizations were reported nation-wide. The most affected demographic group is those ≥65 years, accounting for more than 50% of reported cases.
 Cambodia Reports 8th H5N1 Flu Fatality This Year
Cambodia Reports 8th H5N1 Flu Fatality This Year
26Feb13
Health official in Cambodia have reported the country's eighth fatality this year from H5N1 infection. The victim (35M), from the northeastern province of Kampong Cham, died Monday after eating two ducks that had died due to infection. The total number of confirmed H5N1 cases in Cambodia this year now stands at nine.
This event is worrisome for several reasons. Cambodia has pursued vigorous culling efforts as well as public education efforts. Yet at least one news story out of Cambodia tells of rural villages where “…almost all poultry had died…” weeks before officials were informed or any official culling had been performed. In addition, a Ministry of Health official is quoted as noting that the cases of human H5N1 infection, while rising, do not seem to be connected. From an epidemiological perspective, this is unsettling. Finally, this news comes on the heels of a 2nd H5N1 fatality in China where, as highlighted by Recombinomics, the identity of the H5N1 strains may not be the same in both countries. Further, the sequence from the fatal Chinese isolates show changes in HA shared amongst human cases but absent from any recent poultry sequences.
Since 2003, Cambodia has now aggregated a total of 30 human H5N1 infections, all but three of them fatal and fully one third of which occurred in the first two months of this year. The WHO is reportedly monitoring events closely.
 Cambodia’s H5N1 2013 Death Toll Climbs to Seven
Cambodia’s H5N1 2013 Death Toll Climbs to Seven
21Feb13
The government of Cambodia is reporting yet another victim of H5N1 infection. The news of the most recent victim (2M) follows last week’s death of a three-year-old girl from the same region. This brings the total number of fatalities due to H5N1 infection in Cambodia to seven for just this year. Since the disease was first verified in Cambodia in 2004, a total of 29 human cases have been recorded with 26 associated deaths. Eight of the recorded 29 human cases have occurred just this year. Thus, Cambodia maintains a H5N1 case fatality rate of nearly 90% both this year and historically.
 Seasonal Influenza Continues to Fade Out in U.S.
Seasonal Influenza Continues to Fade Out in U.S.
05Apr13
The latest set of influenza data (see figures at left; for the week ending Mar. 30th; Week 13) released by the CDC today shows a continued “down tick” in most flu-associated parameters, even below threshold levels, while influenza B expands it predominance of residual flu activity. The % of respiratory specimens tested as positive for influenza dropped to 11.3% [down from 16.3% two weeks ago and 13.2% last week] while the % of doctors' visits for ILI remained at 1.8% [from 2.2% two weeks ago and 1.8% last week], but still below the national baseline of 2.2%. Altogether, 7 states and NYC experienced low ILI activity. Fully 43 states experienced only minimal ILI activity. A/H3N2 virus accounts for 58.8% of all antigenically characterized viruses since Oct. 1, 2012 while influenza B accounts for 30.9% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 10.3%.
As in the past 8 weeks, influenza B accounted for over half (74.8%) of typed viruses for week 13 while all influenza A viruses accounted for only 25.2%. Inspection of the stacked column chart (left) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant until the past three reporting weeks. Since early March, influenza B isolates have also fallen. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index has now dropped to 7.4% (compared to 7.5% last week and 7.6% in the prior week). The epidemic threshold for the P&I index for Week 13 is 7.5%.
The number of total influenza-associated pediatric deaths for the season increased to 111 with 1 new fatalities reported for Week 13. The single death was associated with an influenza A viruses for which the subtype was not determined. This is a dramatic decline in the number of influenza-associated pediatric deaths over previous weeks. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 42.3/100,000, up from 41.8/100,000 the week prior. As of the end of Week 13, 11,798 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 180/100,000. The vast majority (>81%) of all influenza- associated hospitalizations were due to influenza A infection.
The season influenza season should continue to ebb over the coming weeks as even influenza B leaves the scene.
 New Avian Influenza Strain Leaves 2 Dead in China
New Avian Influenza Strain Leaves 2 Dead in China
01Apr13 Updated 02Apr13
Chinese health authorities notified the WHO yesterday of three confirmed cases of human infection with a novel avian influenza strain H7N9, according to a Global Alert & Response (GAR) notification issued today by the WHO. Two of the three confirmed cases have been fatal. Laboratory confirmation was obtained by the China CDC on 29 March and additional testing for influenza A(H3N2), A (H1N1)pdm09 and A(H5N1), as well as for novel coronavirus, was negative. The cases eminate out of China's Shanghai and Anhui provinces. On Tuesday, Apr. 2, Recombinomics, quoting an online story from China News, reported another 4 confirmed cases of H7N9 in nearby Jiangsu Province. For three out of the four Jiangsu cases, no obvious link to poultry is apparent nor are there readily evident epidemiological links between the four cases.
As noted in today’s GAR, “…The cases were reported from Shanghai (2 cases) and Anhui province (1 case). All three cases presented with respiratory tract infection with progression to severe pneumonia and breathing difficulties. Disease onset was between 19 February and 15 March 2013. Two of the cases died. The third case is currently in critical condition.” In addition, two sons of one of the Shanghai fatalities were also sick with respiratory illness during the same period and one of the sons has reportedly expired due to pneumonia. Thus, there may well be 2 more “suspected” cases as well. The table, at left, summarizes the confirmed and suspect cases to date.
The WHO-Chinese Influenza Research Center has deposited complete sequences from the first three confirmed cases at GISAID. As noted today in a Commentary at Recombinomics, the sequences from the three human isolates possess a number of sequence signatures for adaptation to humans:
1. All three sequences contain a 15 base pair deletion in their neuraminidase genes. A larger deletion in the same neuraminidase stem region has been linked to human adaptation of H5N1.
2. All three sequences bear the E627K mutation in their PB2 genes. This same mutation was present in the only other known case of fatal H7 influenza infection in humans: a 2003 incident in The Netherlands. Previous studies have demonstrated that the polymerase activity of avian-origin influenza viruses can be dramatically increased in human cells with the PB2 E627K mutation (see for example this link and this link).
3. Two of the three sequences bear the mutation Q226L in their HA genes. This mutation has been linked to higher affinity for human receptors in prior studies on H5N1 transmissivity. Recombinomics has described briefly the prior three H5N1 transmission studies where this mutation enhanced the affinity of the virus for mammalian receptors.
The situation bears close monitoring as the as the potential for the spread of a novel influenza strain among the humans is of great concern. The possibility also exists that this strain of H7N9 is of low pathogenicity in birds but of high pathogenicity in humans.
 So Long and Good Riddance, Influenza A/H3N2!
So Long and Good Riddance, Influenza A/H3N2!
22Mar13
The latest set of influenza data (see figures at left; for the week ending Mar. 16th; Week 11) released by the CDC today indicates a continued shifting of influenza from type A viral infections towards type B and a slight “uptick” in some flu-associated parameters. One state (MI) experienced high activity (up from none last week) while the number of states reporting moderate levels of flu activity remained at 5, as in the preceding week. However, the % of respiratory specimens tested as positive for influenza bounced to 16.3% [down from 17.2% two weeks ago and up from 14.3% last week] while the % of doctors' visits for ILI decreased to 2.2% [from 2.3% two weeks ago and 2.6% last week], at the national baseline of 2.2%. Altogether, 5 states [AL, MS, NV, NJ, and VA ] experienced moderate flu activity while 6 states and NYC experienced low ILI activity. Fully 38 states experienced only minimal ILI activity. A/H3N2 virus accounts for 59.7% of all antigenically characterized viruses characterized since Oct. 1, 2012 while influenza B accounts for 32% of all isolates. Isolates antigenically characterized as 2009 H1N1p are now at 8.3%.
As in the past 5 weeks, influenza B accounted for over half (71.9%) of typed viruses for week 11 while all influenza A viruses accounted for only 28.1%. Inspection of the stacked column chart (left) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more or less constant. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season. As predicted previously, the U.S. could be expected to linger near the epidemic thresholds for a few more weeks.
Other (mainly lagging) indicators of flu activity remained mixed. Most notably, the pneumonia and influenza (P & I) mortality index remained at 7.6% (compared to 7.6% last week and 7.7% in the prior week). The epidemic threshold for the P&I index for Week 11 is 7.5%.
The number of total influenza-associated pediatric deaths for the season increased to 105 with 6 new fatalities reported for Week 11. One of the deaths was associated with A/H1N1p infection, while the other five deaths were due to infection by influenza B. TX has been particularly hard hit with a total of 15 pediatric deaths this season. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 40.5/100,000, up from 39.6/100,000 the week prior. As of the end of Week 11, 11,307 laboratory-confirmed influenza-associated hospitalizations were reported nationwide. The most affected demographic group is those ≥65 years, accounting for 51% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 175/100,000. The vast majority (>83%) of all influenza- associated hospitalizations were due to influenza A infection.
 Update on Novel Human β2c Coronavirus (hCoV-EMC)
Update on Novel Human β2c Coronavirus (hCoV-EMC)
20Mar13
Yesterday, the WHO issued updated surveillance recommendations for human infection by the novel β2c coronavirus (nCoV; hCoV-EMC) that has so far yielded 15 laboratory-confirmed human infections, nine of them fatal. Of note, the WHO is advising clinicians to be watchful for the virus in patients with severe respiratory disease even when other etiological agents are confirmed present. This advice is predicated, in part, by a third cluster of hCoV-EMC cases in the UK that provides “...clear evidence of limited, non-sustained human-to-human transmission…”, though the exact mode of transmission has not been determined. Included in this cluster was a patient who originally tested positive for influenza A but was subsequently found to be co-infected with hCoV-EMC. In addition, the update has specific recommendations for countries where the novel virus has been detected (mainly the WHO Eastern Mediterranean Region) as well as guidelines for investigations to help describe “…critical clinical and epidemiological features of the virus”.
The issue of nCoV surveillance is critical, all the more so since the publication last week in Nature of the identity of the cellular receptor (target) for the new virus. The receptor is an evolutionarily well-conserved protein present on human airway cells known as dipeptidyl peptidase 4 (DPP4; a.k.a in humans as CD26). This enzyme receptor (though the enzymatic activity of DPP4 appears irrelevant to hCoV binding) suggests that direct transmission to and from humans from a variety of species may be possible. This finding heightens concerns that absent proper surveillance with adequate tests, many more cases of human infection may be occurring that are milder in symptomology or mistakenly credited to other infectious agents. Exactly this concern has been vigorously discussed at Recombinomics (see for example, this Commentary). As also noted by Recombinomics, ongoing linkage of hCoV-EMC to related viruses identified in bats has served as a “red herring” that obscures the need for better human surveillance.
 Increased HIV Infection Risk Among Low-SES Hetero-sexuals in the U.S.
Increased HIV Infection Risk Among Low-SES Hetero-sexuals in the U.S.
15Mar13
In this week’s preview edition of the CDC’s Morbidity and Mortality Weekly Report (MMWR), the results of a second round of surveying for HIV prevalence, incidence, and HIV-associated behaviors conducted by the National HIV Behavioral Surveillance System (NHBS) during 2010 were reported. As noted within the report, the “NHBS monitors HIV prevalence and HIV-associated behaviors among populations at high risk for acquiring HIV in 21 metropolitan statistical areas with high prevalence of AIDS. During 2010, NHBS collected data and conducted HIV testing among heterosexuals using respondent-driven sampling, a peer-referral sampling method.” The surveying effort focused on individuals with low socioeconomic status (SES; defined as having a household income (adjusted for household size) at or below the poverty level guidelines or no more than a high school education) since an earlier pilot study showed that “…persons with low SES were more likely than persons with high SES to be infected…”
The major finding in the report is that the HIV prevalence in this low-SES heterosexual population was 2.3% overall, a prevalence roughly 5 times that estimated for the U.S. population over 13 years of age. In addition, a prevalence of 1.1% was found in the sub-pool of respondents who did not report a prior HIV test result. Indeed, among this 1.1% prevalence group, a whopping 43.9% reported that they had never even been tested for HIV infection until they participated in the current survey. Even among the entire survey population, some 25.8% had never previously been tested for HIV.
The study highlights the need for aggressive HIV testing in target populations such as these. As laid out in the accompanying Editorial Note, “A key step to reducing the number of new HIV infections in the United States, as indicated in the National HIV/AIDS Strategy (Link), is to increase the percentage of persons living with HIV who know their serostatus through HIV testing. Persons aware of their HIV infection often take steps to reduce their risk behaviors substantially and can be referred for treatment and care, which can reduce HIV transmission ( link2 ).” The study also highlights the clear socioeconomic divisions that so often underscore disease persistence in the presence of ample medical and public health resources: nearly 92% of the survey participants were African Americans and Hispanics or Latinos.
 U.S. Influenza Recedes to Just Above Epidemic Baselines
U.S. Influenza Recedes to Just Above Epidemic Baselines
08Mar13
The latest set of new data (see figures at left; for the week ending Feb. 23rd; Week 9) released by the CDC today indicates a continued ebbing of influenza from peak levels reached at the end of last year with moderate-levels of activity remaining in just 4 states. The % of respiratory specimens tested as positive for influenza clocked in at 17.2% [up from 16.8% two weeks ago and 16.9% last week] and the % of doctors' visits for ILI decreased to 2.3% [from 2.8% two weeks ago and 2.7% last week], just above the national baseline of 2.2%]. Altogether, 4 states [IL, MI, VT, and VA ] experienced moderate flu activity while 13 states and New York City experienced low ILI activity. A/H3N2 virus accounts for 64% of all antigenically characterized viruses characterized since Oct. 1, 2012 while influenza B accounts for 29% of all isolates. Isolates antigenically characterized as 2009 H1N1p remained at 7%.
However, for the third week in a row, influenza B accounted for over half (64.2%) of typed viruses for week 9 while all influenza A viruses accounted for only 35.8%. Inspection of the stacked column chart (left) shows that since the beginning of the calendar year, most of the decrease in influenza in the U.S. has been due to a decrease in A/H3N2 while influenza B activity has been more constant. This has contributed to the prominent “right shoulder” on the national curves for ILI and % respiratory-specimens-positive-for-influenza this season. Depending upon the persistence of influenza B in the coming weeks, the U.S. could be expected to linger near the epidemic thresholds.
Other (mainly lagging) indicators of flu activity remained elevated. Most notably, the pneumonia and influenza (P & I) mortality index decreased to 7.7% (down from 8.4% last week and 8.6% in the prior week). The epidemic threshold for the P&I index for Week 9 is 7.5%. However, the cyclical seasonal baseline is near its apex (at week 10) and a persistence of influenza B over the coming weeks may keep the P&I index at or near the epidemic threshold.
The number of influenza associated pediatric deaths increased to 87 with 6 new fatalities reported for Week 9. Three of the deaths were associated with H3N2 infection, one was associated with influenza A where sub-typing was not performed, and two deaths were due to infection by influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of laboratory-confirmed flu hospitalizations increased again to 38.5/100,000, up from 36.7/100,000 the week prior. As of the end of Week 9, 10,721 laboratory-confirmed influenza-associated hospitalizations were reported nation-wide. The most affected demographic group is those ≥65 years, accounting for more than 50% of reported cases. The rate of laboratory-confirmed flu hospitalizations for this demographic group exceeded 160/100,000. The vast majority (>84%) of all influenza- associated hospitalizations were due to influenza A infections.
 HIV Infection Tied to Greater Risk of MI
HIV Infection Tied to Greater Risk of MI
05Mar13
The current success of ART in battling HIV to a standstill in infected patients means that HIV patients are living longer and are at-risk for the usual set of age-related diseases, apparently with higher co-morbidity risk. But how much prior HIV infection affects the risk for these diseases is not clear and is difficult to assess. Recently, investigators have turned to military veterans to constitute a suitable cohort for observational study.
A report by Michael Smith at MedPage Today summarizes two studies that show, at least preliminarily, that HIV infection correlates with a two-fold higher risk for myocardial infarction and elevated risk for end-stage renal disease and certain cancers. One of the studies was presented at the ongoing Conference on Retroviruses and Opportunistic Infections (CROI) and the other appears online at JAMA Internal Medicine. The former study examined a cohort of 84,444 veterans (without a history of heart disease) and found that “Although HIV+ adults are at a substantially greater risk of MI, cancer, and ESRD than HIV– adults in care, these age-related co-morbidities occur at similar ages after accounting for traditional risk factors.” The latter study examined a cohort of 82,429 veterans and found that “Infection with HIV is associated with a 50% increased risk of AMI beyond that explained by recognized risk factors.“ As noted in an accompanying “Invited Commentary” for the JAMA article, these studies and other work “…may provide a platform for the development of HIV-specific interventions to reduce this excess MI risk and ensure that the benefits derived from safe, effective, long-term control of HIV replication by ART translate into reduced mortality for all people living with HIV.”
 A Medical First: A Cure in a Pediatric HIV Case
A Medical First: A Cure in a Pediatric HIV Case
04JMar13
The New York Times is reporting a first-ever "functional cure" of HIV in a 26 month-old pediatric case. The infant, born in rural Mississippi to a mother who did not know she was HIV-positive, was subjected to a novel treatment regimen: aggressive anti-retroviral therapy (ART) starting just a mere 30 hours after birth. An oral abstract describing the case was presented today at the 20th Conference on Retroviruses and Opportunistic Infections in Atlanta by Dr. Deborah Persaud (Johns Hopkins University School of Medicine) and colleagues from UMass Medical School, the NIAID, the University of Mississippi Medical Center, and the UCSD/VA San Diego Heathcare System. The 18 month-long ART regimen commenced after positive testing for HIV RNA & DNA (as HIV subtype B) on day 2. Undetectable levels of virus were first detected on day 29 (27 days of treatment).
These results are so important since mother-to-child transmission of HIV is such a major problem. If a mother is known to be infected, prophylactic drug regimens (usually AZT) are typically administered to the newborn. But in this case, Dr. Hannah Gay at the University of Mississippi Medical Center commenced treatment with an aggressive tripartite regimen of anti-retroviral drugs. Extensive testing for HIV when the baby was 5 months-of-age failed to find HIV virus, even in latent reservoirs.
Given the relatively immature state of newborn immune systems, the Times article cites the hypothesis that aggressive ART can be successful in newborns because the virus hasn't had a chance to populate the "hidden reservoirs" that enable the virus to evade host immune responses and drug therapy.
While documented cases of mother-to-child HIV transmission are rare in the U.S (~200 cases per year), the situation is quite different in the developing world where ~300,000 babies were infected in 2011 alone. Today, over 3 million children are infected with HIV worldwide.
While there are multiple reports of HIV patients apparently able to control the virus subsequent to infection (notably the "long term non-progressors"), including at least one pediatric example of HIV clearance, the best most patients can do is battle HIV to a draw employing so-called highly active anti-retroviral therapy [HAART]. There is only one other documented case of curing an HIV infection: a German patient suffering both from leukemia and HIV who received a bone-marrow transplant from a donor whose cells were genetically missing a key receptor for HIV infection.
These results constitute an exciting medical finding and should catalyze many additional studies to ascertain whether early detection and aggressive treatment can save the lives of young children and potentially avoid a lifetime of HAART.
 Flu Wave Continues to Ebb, But Still Plenty of Flu Around
Flu Wave Continues to Ebb, But Still Plenty of Flu Around
22Feb13
The latest set of new data (see figures at left; for the week ending Feb. 16th; Week 7) released by the CDC today indicates a continued abatement from peak levels of influenza with moderate-to-high levels of activity remaining in just 16 states. Down activity indicators include the % of influenza-positive tests of respiratory specimens [down from 19.7% to 16.8%] and the % of doctors' visits for ILI decreased from 3.2 to 2.8% [though still above the national baseline of 2.2%]. Altogether, 3 states experienced high ILI activity, 13 states and New York City experienced moderate ILI activity. A/H3N2 virus accounts for 62.7% of all antigenically characterized viruses while influenza B accounts for 30% of all isolates characterized since Oct. 1, 2012. Isolates antigenically characterized as 2009 H1N1p fell to 7.3%.
As with last week's report, several (mainly lagging) indicators of flu activity remained elevated. Most notably, the pneumonia and influenza (P & I) mortality index decreased to 8.6% (down from 9.1% in the prior week). The epidemic threshold for the P&I index for Week 7 is 7.5% The number of influenza associated pediatric deaths increased to 78 with 14 new fatalities reported last week. This is a substantial increase from the 5 reported the week prior. Three of the 14 deaths were associated with H3N2 infection, two were associated with influenza A where subtyping was not performed, and six deaths were due to infection by influenza B. Strikingly, two pediatric deaths were associated with 2009 H1N1p infection which constitutes a small number of overall influenza infections typed in the U.S. this season (<10%). The remaining pediatric fatality was associated with influenza A and influenza B infection. Finally, the season-to-date [from Oct. 1, 2012) rate of flu hospitalizations jumped again increased to 34.2/100,000, up from 32.1/100,000 the week prior. As of the end of Week 7, 9,531 laboratory-confirmed influenza-associated hospitalizations were reported nation-wide. The most affected demographic group is those ≥65 years, accounting for more than 50% of reported cases.
 2009 H1N1p Spreads its Wings (Again)
2009 H1N1p Spreads its Wings (Again)
21Feb13
The number of cases of swine flu [2009 H1N1p] continues to expand rapidly in the Mideast and South Asia. A number of local news reports from the affected regions highlight increasing concern as the number of cases swell. For example, New Delhi has now reported a total of 570 confirmed cases of swine flu infection this year. This compares to a total of 78 cases for all of last year. Health officials in neighboring Northern Indian states (e.g. Haryana, Punjab, and Rajasthan) have been cited as describing the swine flu situation there as “alarming”, notably in Rajasthan. Elsewhere in India, recent reports describe a mounting death toll and a rapidly increasing number of confirmed cases of 2009 H1N1p infections (for example, see the following links: link1, link2, and link3).
India is not the only area experiencing difficulties with 2009 H1N1p (for example, see the following links: link4 and link5). The most recent update from the WHO [dated 15Feb13] notes that “Influenza A, mainly A(H1N1)pdm09, was reported as the dominant virus in countries in northern, eastern, and central Europe, including Austria, the Czech Republic, Germany, and the Russian Federation, while influenza B was reported as the dominant virus in some countries in the southern and western parts of the region, including France, Ireland, Italy, Spain, and United Kingdom. Between these areas, co-circulation of A(H1N1)pdm09, A(H3N2), and influenza B was reported.” In addition, the WHO notes that “The proportion of influenza-positive sentinel specimens increased to reach the highest level so far this season [2012-2013], 52 percent (1541/2949), increasing from about 40 percent over the preceding 3 consecutive weeks. The proportion of hospitalized cases of severe acute respiratory infection (SARI) that were positive for influenza also continued to increase, and was mainly due to influenza A(H1N1)pdm09 viruses.”
Interestingly, a “ skyrocketing” number of cases (155) of 2009 H1N1p have now been reported in Edmonton, Canada, while nearby Calgary has tallied 15 cases including one fatality. As in the United States, influenza in Canada this season has largely been the result of H3N2 and influenza B infections. These 2009 H1N1p infections in Canada have occurred against a backdrop of coverage by the current flu vaccine.
These observations open the possibility that the 2009 H1N1p virus is just now beginning to surge (once again) and that another wave of influenza may be possible in North America, this time arising from a resurgent pandemic virus.
 Pediatric Influenza-associated Mortality Jumps in Week Seven
Pediatric Influenza-associated Mortality Jumps in Week Seven
21Feb13
In today’s weekly Notifiable Diseases and Mortality Tables, the CDC is reporting 14 pediatric influenza-associated deaths for the week ending February 16, 2013. This is a number significantly higher than the 5-year weekly average of 4 fatalities. The total number of pediatric influenza associated deaths for 2013 now stands at 60. States reporting fatalities for the week ending February 16 are: NY (2), IN (2), IL (1), MN (2), FL (1), AR (1), TX (1), NM (2), UT (1), NYC (1). More details on influenza statistics for week seven should be published tomorrow.
 Flu Wave Ebbs Nationally, But Remains at Above Epidemic Levels
Flu Wave Ebbs Nationally, But Remains at Above Epidemic Levels
15Feb13
The latest set of new data (see figures at left; for the week ending Feb. 9th; Week 6) released by the CDC indicates a continued abatement from peak levels of influenza with moderate-high levels of activity remaining in a little over half the states. Down activity indicators include the % of influenza-positive tests of respiratory specimens [now below 20% at 19.7%] and the % of doctors' visits for ILI decreased from 3.6 to 3.2% [though still above the national baseline of 2.2%]. Altogether, 11 states and New York City experienced high ILI activity [down from 19 + NYC the prior week]. A/H3N2 virus accounts for 62% of all antigenically characterized viruses while influenza B accounts for 30% of all isolates characterized since Oct. 1, 2012. Isolates antigenically characterized as 2009 H1N1p were at 8%.
However, several (mainly lagging) indicators of flu activity were up last week. Most notably, the pneumonia and influenza (P & I) mortality index climbed to 9.1% (from 9.0% in the prior week). This is the 4th week in a row that the P&I index was at or above 9%. The epidemic threshold for the P&I index for Week 6 is 7.5% The number of influenza associated pediatric deaths increased to 64 with 5 new fatalities reported last week. This is a substantial decrease from the 19 reported the week prior. However, only 1 of the 5 deaths was associated with H3N2 infection; four were due to infection by influenza B. Finally, the season-to-date [from Oct. 1, 2012) rate of flu hospitalizations jumped last week to 32.1/100,000, up from 29.8/100,000 the week prior. As of the end of Week 6, 8,953 laboratory-confirmed influenza-associated hospitalizations were reported nation-wide. The most affected demographic group is those ≥65 years, accounting for more than 50% of reported cases.
While the contribution of influenza to ILI in the US wanes, PAHO (a regional office of the WHO) is reporting a spike in RSV infections in Canada and that RSV infections are already increasing in the US.This latter event may cause a rise in ILI over the coming weeks but with a corresponding decrease in the % of respiratory specimens testing positive for influenza.
 Short Telomeres Linked to Contracting the Common Cold
Short Telomeres Linked to Contracting the Common Cold
19Feb13
An article appearing on MedPage Today covers a recent report in the literature from investigators at Carnegie Mellon University that establishes a correlation between an increased rate of infection by rhino viruses and shorter telomeres on CD8+CD28- T cells. Telomeres are regions of repetitive nucleic acids at the end of each chromatid that serve to protect the end of the chromosome from degradation. Each time a cell divides the telomeres shorten since the enzymatic apparatus for their replication cannot proceed past the end of the chromatid. An enzyme known as telomerase can extend telomeres but this enzyme is present only in select cells, such as stem cells. Thus, telomere length can be taken as a measure of cell age and prior studies have led to the suggestion of a general correlation between telomere length and age-related functional decline.
In the present study, published in the Journal of the American Medical Association, the investigators studied telomere length on 152 adults aged 18 to 55 years of age. Patients were given nasal drops containing either control or rhinovirus 39 and subsequently monitored for five days for “Infection (virus shedding or 4-fold increase in virus-specific antibody titer) and clinical illness (verified infection plus objective signs of illness).” Four distinct sets of leukocytes (including PBMCs and CD4+ T cells) were then evaluated for telomere length. Only CD8+CD28- T cell telomere length was associated with greater risk of infection and clinical illness.
There is other evidence to support a possible causative link between telomere length and viral infection. A prior report had examined the same 4 leukocyte subsets in healthy adults and had found “...that CD8+CD28- T cells are replicatively senescent cells, they had the lowest telomerase activity and shortest telomere length.” More specifically, it has also been previously reported that sustained CD28 expression delays features of replicative senescence (e.g. “enhanced telomerase activity, increased overall proliferative potential, and reduced secretion of pro-inflammatory cytokines” ) in CD8 T cells. Perhaps not surprisingly then, the abundance of CD8+CD28- T cells correlates with accelerated AIDS progression (see link1). Continued research on the correlations and potential causality of immunosenescence and viral infections could lead to diagnostic biomarkers of disease and even new therapies.
 Recently Discovered Virus Claims Its Spot Among U.S. Pediatric Respiratory Infections
Recently Discovered Virus Claims Its Spot Among U.S. Pediatric Respiratory Infections
15Feb13
In a a new article appearing in the New England Journal of Medicine, investigators from the New Vaccine Surveillance Network have reported the results of a prospective surveillance study of a new respiratory virus discovered only in 2001.
The virus is human metapneumovirus (HMPV), a paramyxovirus [ssRNA] virus related to measles, mumps, and respiratory syncytial viruses, as well as human parainfluenza virus 1-4, though its closest neighbor is avian metapneumovirus (AMPV) subgroup C. As noted by the investigators in their article, HMPV “…is associated with acute respiratory illness among infants and children worldwide. In addition, HMPV causes acute respiratory illness and results in hospitalization among older adults and persons with underlying chronic conditions, including asthma, cancer, and chronic obstructive pulmonary disease.”
The present study illuminates the disease-burden of metapneumovirus among children under five, since prior work was retrospective and was missing asymptomatic controls. In this case, data was collected from region surrounding three US cities over six years (2003-2009) and involved over 12,000 children. New types of data were also collected including rates of hospitalization, as well as emergency department and outpatient visits.
It was found that “HMPV infection is associated with a substantial burden of hospitalizations and outpatient visits among children throughout the first 5 years of life, especially during the first year. Most children with HMPV infection were previously healthy.” Specifically HMPV was detected in 6% of pediatric inpatients and 7% of pediatric outpatients. Moreover, the rate of HMPV hospitalizations for children less than five years of age was one per 1,000, similar to that for influenza but below that due to RSV (3/1,000). The authors estimate, based on census data, then approximately 20,000 HMPV hospitalizations occur annually for children less than five years of age.
The study underscores the importance of the need for a diagnostic test for HPMV, especially in light of the shared symptomology with RSV and influenza. In addition, there is a clear impetus for an effective vaccine.
 More H5N1 Fatalities in Asia
More H5N1 Fatalities in Asia
13Feb13
Two more individuals have died in Asia from H5N1infection. Xinhua News Agency, China’s official news agency citing government Health Ministry officials, is reporting that one of two individuals recently confirmed with H5N1 infection has died. The patient (21F) from Guiyang, China passed away today from multiple organ failure, 11 days after first showing influenza symptoms. The other individual (31M) with confirmed H5N1 infection is also from Guiyang and is reported to be in critical condition. Interestingly, cited “epidemic control experts" have not found any indication that either patient had close contact with birds nor is there any apparent epidemiological connection between the two cases.
Meanwhile, Cambodia has registered its seventh case and sixth death this year from H5N1. The details were outlined in a joint statement from the WHO and Cambodia’s Ministry of Health. The victim (3F) was tested positive for H5N1 on 11Feb after developing a fever and rash on 03Feb. The child reportedly had contact with poultry prior to being infected. As noted in the joint statement, “Globally since 2003, there have been 619 laboratory confirmed human cases of avian influenza with 366 related deaths.” But Cambodia has suffered much more with a total of 28 confirmed cases and 25 deaths, most in children.
 Recently Discovered Virus Claims Its Spot Among U.S. Pediatric Respiratory Infections
Recently Discovered Virus Claims Its Spot Among U.S. Pediatric Respiratory Infections
15Feb13
In a a new article appearing in the New England Journal of Medicine, investigators from the New Vaccine Surveillance Network have reported the results of a prospective surveillance study of a new respiratory virus discovered only in 2001.
The virus is human metapneumovirus (HMPV), a paramyxovirus [ssRNA] virus related to measles, mumps, and respiratory syncytial viruses, as well as human parainfluenza virus 1-4, though its closest neighbor is avian metapneumovirus (AMPV) subgroup C. As noted by the investigators in their article, HMPV “…is associated with acute respiratory illness among infants and children worldwide. In addition, HMPV causes acute respiratory illness and results in hospitalization among older adults and persons with underlying chronic conditions, including asthma, cancer, and chronic obstructive pulmonary disease.”
The present study illuminates the disease-burden of metapneumovirus among children under five, since prior work was retrospective and was missing asymptomatic controls. In this case, data was collected from region surrounding three US cities over six years (2003-2009) and involved over 12,000 children. New types of data were also collected including rates of hospitalization, as well as emergency department and outpatient visits.
It was found that “HMPV infection is associated with a substantial burden of hospitalizations and outpatient visits among children throughout the first 5 years of life, especially during the first year. Most children with HMPV infection were previously healthy.” Specifically HMPV was detected in 6% of pediatric inpatients and 7% of pediatric outpatients. Moreover, the rate of HMPV hospitalizations for children less than five years of age was one per 1,000, similar to that for influenza but below that due to RSV (3/1,000). The authors estimate, based on census data, then approximately 20,000 HMPV hospitalizations occur annually for children less than five years of age.
The study underscores the importance of the need for a diagnostic test for HPMV, especially in light of the shared symptomology with RSV and influenza. In addition, there is a clear impetus for an effective vaccine.
 Recombinomics Reports sH3N2 HA Variant Present in US Isolates Collected in 2013
Recombinomics Reports sH3N2 HA Variant Present in US Isolates Collected in 2013
03Feb13
Recombinomics (www.recombinomics.com) reported yesterday that the CDC has deposited (at GISAID) the first U.S. 2013 H3N2 sequences showing a influenza virus hemagglutinin (HA; H3) with a mutation (T128A) that abolishes a protein-linked glycosylation site. Specifically, the mutation from a threonine residue to alanine disrupts the canonical tripeptide consensus sequence (Asn-X-Ser/Thr; where X is any amino acid save proline) required, but not sufficient, for N-glycosylation of mammalian proteins. The influenza virus hijacks the mammalian protein synthesis machinery, including the host post-translational modification apparatus, to replicate its own proteins. This is not only efficient for the virus but also provides another mechanism of immune evasion as the virus literally cloaks itself in “host” structures.
The sequence, A/Virginia/03/2013, was collected from a 76 year-old female early in January and is closely related to a sequence previously collected this season, A/Iowa/14/2012, that bears the same mutation and has already been designated a “low reactor” by the CDC. Low reactor status indicates that antibodies engendered by the current vaccine poorly recognize this viral specimen. Therefore, prior administration of the vaccine is less likely to convey meaningful protection when individuals are infected with the “low reactor” strain.
The potential loss of a HA N-glycosylation site might normally be thought to enhance the immunogenicity of the virus, since N-glycans are thought to mask a significant portion of the surrounding HA molecular surface. Indeed, the addition of N-linked sites on the HA surface has previously been associated with the adaptation (and loss of virulence) of pandemic viruses in humans over time, as in the case of 1918 pandemic H1N1. In the present case, however, the loss of an N-linked glycan might result in the exposure of a more immunodominant epitope that effectively decoys the human immune response and conveys “low reactor” status to the mutant virus.
Of course, the other possibility is that the N-glycosylation site at Asn-126 was never occupied and that the observed mutation disrupts an important and dominant vaccine epitope on the HA surface. Deciding between these two possibilities must await, among other things, data on the N-glycan site occupancy for the vaccine strain H3N2.
As noted in the Recombinomics Commentary, this is not the first time this season that this mutation has been found amongst deposited sequences originating either in the U.S. or elsewhere in the world (T128A has been found in isolates from England, Denmark, Greece, Hong Kong, Senegal, and France, as well as the U.S.). The CDC has recently deposited 6 additional sequences from isolates collected in December and 4/6 HA sequences carry T128A. It will be of considerable interest to follow the chronology of vaccine effectiveness, initially marked at 55% in the U.S., and compare it to the relative abundance of T128A mutants in the viral HA sequences deposited by the CDC.
 Breathprints Identify Lung Infections in Mice
Breathprints Identify Lung Infections in Mice
28Jan13
According to a news article on Medwire News, a team of investigators led by Jane Hill at the University of Vermont-Burlington have used mass spectrometry to identify significant differences in the volatile organic compounds (VOCs) present in the exhaled breath of mice infected with Pseudomonas or Staphylococcus, as compared to the breath of non-infected mice. Such “breathprints” could be eventually used to detect whether patients have a bacterial respiratory infection, a notoriously difficult task in the clinic where culturing a pathogen from patients is time-consuming and frequently ambiguous.
As just reported in the Journal of Breath Research, the investigators used secondary electrospray ionization mass spectrometry (SESI – MS) to qualitatively assess VOCs in vivo. Most intriguingly, the team found that the breathprints of mice infected with Pseudomonas differed from those from mice infected with Staphylococcus. Moreover, the investigators found that as SESI – MS could distinguish between infections in mice of two different strains of Pseudomonas. Finally, it was “…observed that only 25–34% of peaks are shared between the in vitro and in vivo SESI-MS fingerprints.”
The eventual development of new diagnostic tools using technologies such as SESI – MS promises to revolutionize the diagnosis of respiratory infections. The vast majority of debilitating lower respiratory tract infections is caused by bacterial, viral, or fungal pneumonia and treatment of patients is frequently hampered by the lack of fast and reliable in situ diagnostic tests that can determine the offending pathogen.
 WHO: Two More Human Deaths from H5N1 in Cambodia
WHO: Two More Human Deaths from H5N1 in Cambodia
29Jan13
The WHO is today reporting two additional cases of human H5N1 in Cambodia. The patients, girls aged 17 months and nine years old, were confirmed positive for the H5N1 virus earlier this month and died yesterday. In both cases, there is evidence of recent deaths among poultry in their respective villages. The monthly total of H5N1 human infections in Cambodia now stands at a total of five, with four fatalities. This number exceeds the total number of H5N1 cases in Cambodia all of last year.
The relatively high number of H5N1 infections in Cambodia so far this year is worthy of careful watch, especially as the country heads towards the Chinese New Year, which starts February 10th. This holiday presents a golden opportunity for an increase number of infections since it is a time when many chickens, some of them possibly infected, make their way to market and possibly enhance the probability of human infection. To support this possibility, local health officials are pursuing a number of measures, including the additional calling of poultry suspected of being infected.
 Flu Activity Persists While the P&I Index Climbs Steeply
Flu Activity Persists While the P&I Index Climbs Steeply
25Jan13
Data released today by the CDC shows that influenza activity remained elevated in the United States, but was decreasing in some areas, with forty-seven states reporting widespread geographic influenza activity. Most notable among the reported data was the large spike in the proportion of deaths attributed to pneumonia and influenza (P&I), which is well above the epidemic threshold, standing at 9.8%. As noted in a Commentary at Recombinomics, "...the 9.8% level has not been seen in the prior years displayed and which is also true for the steep slope. The 9.8% level is the highest seen since 2003, when an H3N2 strain, A/Fujian/411/2002, produced a large number of deaths in those over 65 as well as an alarming pediatric death rate."
In the current data set, eight more influenza-associated pediatric deaths were reported since the week prior, raising the official number of nfluenza-associated pediatric deaths reported during the 2012-2013 season to 37. Of the eight newly attributed pediatric deaths, two were associated with influenza A viruses for which the subtype was not determined and six were associated with influenza B viruses.
An aggregate total of 6,191 laboratory-confirmed influenza-associated hospitalizations have now been reported this season, a rate of 22.2 per 100,000 population. The most affected group is those ≥65 years, accounting for 50% of reported cases.
 WHO Declares Dengue the Fastest-Growing Tropical Disease.
WHO Declares Dengue the Fastest-Growing Tropical Disease.
16Jan13
In a statement issued this week, the WHO declared dengue as the fastest-growing tropical disease in the world, with an estimated 50 million cases each year. Dengue, which was first found just over 60 years ago in three countries, has increased its geographical spread to over 120 countries and all inhabited continents. Over the decades, the number of cases has continued to increase and officially over 2 million cases of dengue are reported each year. In other words, dengue has registered a 30-fold increase in disease incidence over the past 50 years.
But according to a recent story published by Reuters, the WHO now estimates that the actual number of cases of dengue is more like 50 million and may be as high as 100 million cases a year. Moreover, the disease now represents a pandemic threat and is overtaking malaria as the mosquito-borne disease with the greatest reach. The “exponential explosion” of dengue is believed due to climate change, globalization, and changes in the geographical distribution of the mosquito vectors, Aedes aegypti and Aedes albopictus. Dengue now has a global reach.
There are currently no therapeutic treatments for dengue. A number of vaccine candidates are under development. The most mature program is that led by Sanofi SA which, in clinical trials published last year, appears safe but is only about 30% effective.
 Rotavirus Vaccination Can Protect Familial Bystanders
Rotavirus Vaccination Can Protect Familial Bystanders
24Jan13
One of the most interesting public health insights of recent years, translated into policy as vaccination recommendations to the public, has been the realization that more aggressively vaccinating children against influenza virus can significantly impact the level of disease in older adults. Now, a newly published study indicates that the same principle maybe operative when vaccinating children against rotavirus.
In a study just published in Clinical Infectious Diseases and reported by MedPage Today, a group of investigators at Emory University found a reduction in the relative percentage of rotavirus positive stool cultures (of between 42.5 and 49.3%) and an absolute decline from 4.35% to 2.24% in adult samples obtained at a single medical center before and after the widespread use of the pediatric vaccine. A marked reduction in rotaviral disease in both the vaccinated and unvaccinated pediatric populations shortly after the FDA approved the road attack vaccine in 2006 has been well documented already.
These are early results, limited by a number of factors and subject to further refinement through additional study. However, the possibility that vaccinating children can beneficially impact the adult population against rotavirus disease is an exciting development that warrants further study.
 High Flu Activity Persists But May Be Decreasing in the East
High Flu Activity Persists But May Be Decreasing in the East
08Feb13
The latest set of new data (see figures at left) released by the CDC indicates a continued decrease from peak levels of influenza while high levels of activity remain in select regions. ILI activity eased further in the East and was attenuated in the West though high levels of ILI activity remain entrenched in New York City and New Jersey, Michigan, and Texas, Oklahoma, and Kansas. Altogether, 19 states and New York City experienced high ILI activity and the proportion of outpatient visits for ILI was 3.6%, still above the national baseline of 2.2%. A/H3N2 virus accounts for 63% of all antigenically characterized viruses while influenza B accounts for 31% of all isolates characterized since Oct. 1, 2012.
Most notably, the pneumonia and influenza (P & I) mortality index remained much above the epidemic threshold at 7.3% though it was down again from a peak value of 9.8% two weeks ago and 9.4% last week. The number of influenza associated pediatric deaths jumped to 59 with 14 new fatalities reported just last week. Three of the 14 deaths were associated with H3N2 infection, four were associated with infection by undetermined influenza a virus, at and seven were due to infection by influenza B. This week’s influenza associated pediatric deaths are the highest recorded yet this season. Recombinomics has tabulated an additional 11 influenza associated pediatric deaths not included in the CDC figures but reported in the media and reports from state health labs.
 High Flu Activity Persists But May Be Decreasing in the East
High Flu Activity Persists But May Be Decreasing in the East
01Feb13
Data released today by the CDC shows that influenza activity remains elevated in the United States, but potentially is decreasing in some regions. Forty two states reporting widespread geographic influenza activity, down from 47 the week before.
In the current data set, eight more influenza-associated pediatric deaths were reported since the week prior, raising the official number of nfluenza-associated pediatric deaths reported during the 2012-2013 season to 45. Of the eight newly attributed pediatric deaths, five were associated with A/H3N2, one was associated with influenza A viruses for which the subtype was not determined, and two were associated with influenza B viruses.
An aggregate total of 7,224 laboratory-confirmed influenza-associated hospitalizations have now been reported this season, a rate of 25.9 per 100,000 population, up from 22.2 per 100,000 population the week before. The most affected group is those ≥65 years, accounting for 50% of reported cases.
The P&I Mortality Index for 122 cities came in at a very high of 9.4%. This percentage was above the epidemic threshold of 7.4% for week 4. This is the second week in a row that the P&I Index was above 9% (9.8% last week; see graph at left).
 And Lest We Forget Pandemic H1N1
And Lest We Forget Pandemic H1N1
29Jan13
While attention is naturally focused on this year’s intense seasonal influenza (A/H3N2) outbreak, norovirus, and troubling news concerning H5N1 in Cambodia, a spate of other recent reports serves to remind us that pandemic H1N1 (2009 pH1N1) has not yet left the world stage.
The 2009 pH1N1 pandemic was officially declared over by the WHO in August 2010. And confirmed cases of 2009 pH1N1 infection are relatively infrequent in North America and Europe this season, the virus having been displaced by the H3N2 virus. Similarly, the southern hemisphere experienced relatively minor problems with 2009 pH1N1 last year during their winter season. However, a recent study put the global pH1N1 infection rate after the first year of exposure at 24%, leaving large populations under exposed and under-vaccinated. Thus, other parts of the world are still dealing with troubling outbreaks of the 2009 pH1N1 virus.
A report out today from Tel Aviv sites over 700 pH1N1 infections this season, resulting in 25 deaths in recent weeks in the Occupied Palestinian Territory. India is dealing with an outbreak of 2009 pH1N1 this season (for example, see the following links: link1, link2, link3, and link4). China has already reported 5 deaths due to pH1N1 in Beijing this year. A swath of other countries, from Jordan to Bosnia, have recently reported outbreaks of 2009 pH1N1.
What do all of these reports mean? Primarily, these reports underscore the need for continued surveillance and vigilance. As a zoonotic pathogen, influenza is constantly undergoing alterations via recombination and reassortment with other influenza strains. These are the mechanisms by which deadly new influenza strains arise. So in this very active flu season, it is best to remind us to survey a broad horizon and not to focus solely on local, immediate problems.
 Candidate Dengue Vaccine Shows Promise in Phase 1 Study
Candidate Dengue Vaccine Shows Promise in Phase 1 Study
23Jan13
A press release out today from the NIH has announced the a candidate dengue vaccine developed by scientists at the NIH has been found to be safe and generate a strong immune response in recipients participating in a phase 1 clinical trial sponsored by the NIAID. The results of the trial have just been published online in the Journal of Infectious Diseases.
The WHO estimates that 50 to 100 million cases of dengue occur worldwide every year with a resulting 500,000 hospitalizations of patients with more severe forms of the disease, most of them children. One third of the world’s population is chronically at risk each year for this viral infection and there are currently neither therapies nor vaccines for this disease.
Dengue fever can because by any of four related viruses, and the NIH’s vaccine candidate, Tetra-Vax DV, is composed of a live attenuated form of each virus. In the Phase I trial, a randomized, placebo-controlled study, the safety and immunogenicity of four different admixtures of a live attenuated tetravalent vaccine were evaluated in 113 naïve adults. Participants were randomized into four groups of 28. Within each group, 20 individuals received a single s.q. injection of one of the tetravalent candidate vaccine combinations, and eight others received placebo.
As described in the press release, "The researchers found that all four candidate vaccine combinations induced antibody responses against each of the dengue viruses. However, one vaccine combination, TV003, appeared to induce the most balanced antibody response against the dengue viruses. A single dose of TV003 resulted in an antibody response to all four dengue viruses in 45 percent of participants and against three of the four viruses in an additional 45 percent. Overall, an immune response to at least three viruses was seen in 90 percent of vaccinees given TV003.
All of the candidate LATV vaccines were also found to be safe: no participants experienced fever or dengue-like illness after vaccination, though 64% of recipients did develop a faint rash at the site of injection.
As also noted in the NIH press release, "...TV003’s inexpensive production cost—less than $1 per dose—is critical to its potential use in developing countries, noted Dr. Whitehead. Manufacturers in Brazil, India and Vietnam—countries where dengue is prevalent – have licensed the vaccine technology for production and further evaluation. Phase II trials to evaluate the safety of TV003 and its capacity to create an immune response will begin soon in Brazil and Thailand."
This news comes on the heels of disappointing clinical results for a more advanced dengue candidate vaccine last fall and provides additional hope for an eventual effective vaccine.
 CDC: A New Strain of Norovirus Takes Over
CDC: A New Strain of Norovirus Takes Over
25Jan13
In a new Morbidity and Mortality Weekly Report [MMWR] released today, the CDC has announced that a new strain of norovirus, known as GII.4 Sydney, is sweeping the globe, including the United States. The new strain was first identified last March in Australia. During the period of September–December 2012, a total of 141 (53%) of the 266 norovirus outbreaks reported to the CDC were caused by GII.4 Sydney.
Sometimes mistakenly called the stomach flu, norovirus is the leading cause of epidemic gastroenteritis in the U.S., causing bouts of vomiting and diarrhea for 2 to 3 days. The virus is best known for being highly contagious and spreading quickly amongst humans in close confinement, such as cruise ships and nursing homes. Each year, noroviruses viruses cause an estimated 21 million illnesses and 800 deaths [ ].
As noted in the MMWR, “Noroviruses belong to the family Caliciviridae and can be grouped into five genogroups (GI through GV), which are further divided into at least 34 genotypes. Human disease primarily is caused by GI and GII noroviruses, with most outbreaks caused by GII.4 strains. During the past decade, new GII.4 strains have emerged every 2–3 years, replacing previously predominant GII.4 strains. Emergence of these new norovirus strains has often, but not always, led to increased outbreak activity. For example, the previously dominant GII.4 New Orleans strain was not associated with increased norovirus outbreak activity in the United States.”
 WHO: Two Cambodians Die from H5N1 Bird Flu
WHO: Two Cambodians Die from H5N1 Bird Flu
25Jan13
According to a news report in the Terra Daily, the World Health Organization reported last Friday that two individuals have died from H5N1 infection in Cambodia. The two victims, a 15-year-old girl and a 35-year-old man, passed away after preparing infected chicken. In addition the agency reported the existence of a pediatric case earlier in the month, but that patient later recovered. In total, there have been 24 reported cases of HIV in one in Cambodia since 2003 and all but three of the cases were fatal.
The WHO has reported that, worldwide as of 16Jan13, there have been a total of 610 laboratory-confirmed human cases of influenza A(H5N1) virus infection from 15 countries, of which 360 died. This latest assessment also notes that... “Recent poultry outbreaks in Indonesia have been attributed to influenza virus A (H5N1) clade 2.3.2.1. This clade has not been previously detected in Indonesia, although it has been circulating for some years in poultry and has been isolated from a few human cases with H5N1 infection in other countries.”
 Flu Activity Persists At High Levels
Flu Activity Persists At High Levels
18Jan13 Updated 21Jan13
The flu season continues unabated according to the latest data from the CDC (see the data at left, courtesy of the CDC). Every state, except for Tennessee and Hawaii, has reported widespread flu activity. Some are hoping that recent reductions in ILI visits and in the number of flu positive tests reported to the CDC may hearld that the worst is past.
However, Tthe fraction of deaths nationwide attributed to pneumonia and influenza (the P&I index) spiked to 8.3%, above the epidemic threshold of 7.2% for the second week in a row. Even more notable was a sharp increase in the hospitalization rate for laboratory-confirmed influenza that climbed to 18.8 per 100,000 people, up from 13.3 per 100,000 the week before. For individuals 65 or older, the rate jumped to 82 per 100,000.
The number of pediatric deaths due to influenza also jumped to 29 with nine additional fatalities added just the preceding week. Moreover, Recombinomics is citing other pediatric deaths this season that could mean the actual pediatric death toll is 41 with two ther cases still under investigation. Regardless, the nine fatalities reported for the week ending Jan. 12 is the highest since the peak of the 2010-2011 season, as also noted in the Recombinomics Commentary.
Finally, data from select states indicates that flu activity is still on the upswing in certain geographical regions. For example, Recombinomics is citing data from Minnesota showing a dramatic uptick in flu-related hospitalizations and fatalities over the past two weeks (with 56 of the 60 reported fatlities this season reported in weeks 1 and 2 of this year).
The primary culprit in the U.S. has been and remains influenza A, especially H3N2. This is in contrast ot other regions of the globe (Northern climes) where the 2009 H1N1p strain is more prevalent.
As reported by Todd Neale at MedPage Today, the Director of the CDC, Thomas Frieden, told reporters in an allied conference call that …"We expect to see both the number and the rates of both hospitalizations and deaths rise further in the next week or so as the flu epidemic progresses and people have the complications of the illness that they developed in the past."
 A “Molecular Timer” for Influenza
A “Molecular Timer” for Influenza
19Jan13
An article just out in Cell Reports describes the careful chronological balance that influenza must maintain when it infects a cell. On the one hand, the virus needs sufficient time to produce as many daughter virions as possible while, on the other hand, it risks getting trounced by the host immune system if it overstays its welcome.
Influenza manages this balancing act through a weak differential splicing event in transcripts of segment 8 (the NS segment), which is best known for encoding the multifunctional NS1 protein, the major viral counter against host cell responses to infection. Alternative splicing of the NS1 mRNA ultimately produces another multifunctional protein, termed NS2. NS2 is also known as nuclear export protein (NEP) due to its role in the export of viral ribonucleoprotein complexes from the host cell nucleus, a crucial step in the ultimate production of daughter virions. In addition, NEP, through interaction with the cellular F1Fo ATPase, plays a key role in the viral budding process and in regulating the accumulation of viral RNA species, potentially switching from early viral transciption to replication (see the recent article by Paterson & Fodor for an excellent review of NEP functions).
In their newly published paper in Cell Reports, Chua et al. employed a total of 5 complementary strategies to better define the roles of NS1 and NEP during virus infection, including the use of microRNA targeting to silence NS1 without impacting NEP levels. “Surprisingly, these strategies all demonstrated that NEP accumulation plays a more substantial role during in vivo virus infection than the sustained expression of the IAV interferon antagonist protein, NS1.” Most especially, employing the host splicing apparatus through a weak 5’ splice site allows the virus to generate a “molecular timer” via the slow accumulation of NEP, an accumulation that mediates the switch from transcription to viral replication. As noted by the investigators, “Taken together, the virus has exploited the predictable nature of the cell to establish a molecular timer and successfully coordinate the processes of infection.”
The ability of influenza to continually surprise us is confirmed yet again. This work not only deepens our understanding of how the influenza virus makes the most use of its limited genomic assets in interacting with a host to regulate its own life cycle but also portends new molecular targets for therapeutic intervention. It was already known that disruption of NEP’s nuclear export signal results in the failure of the virus to replicate. New targets suggested by this study, such as blocking the over production of NS1 or targeting the weak splice site that generates NEP, could yield powerful new therapies against influenza through disruption of the viral life cycle.
 Proposed HIV Clinical Trial in the Crosscurrents of Controversy.
Proposed HIV Clinical Trial in the Crosscurrents of Controversy.
16Jan13
The recent discovery of broadly neutralizing anti-HIV monoclonal antibodies has catalyzed a drive to conduct clinical trials in order to ascertain the safety and efficacy of these as biologics. But now, according to a news report by Meredith Wadman appearing today in Nature News and Comment, one of the proposed studies is drawing considerable criticism and debate.
At the heart of the issue is a public health “…conundrum: breast milk protects infants from pneumonia and gastroenteritis, major killers in developing countries, but the milk can also transmit HIV.” As reported in the Nature News story, it has been estimated that roughly 150,000 new pediatric HIV infections in sub-Saharan Africa were acquired through breast-feeding in 2011. The problem is so severe that the WHO recommends all HIV-positive women breast-feed their infants and that both mother and baby take antiretroviral (ARV) therapy. While the cost of ARV therapy in the developing world is less than $200 ($USD) per year per patient, there are still problems. Even with these orally available drugs, there is still a breakthrough rate of 2 to 5% in babies at six months of age.
The proposed trial was to study the safety and efficacy of a human monoclonal antibody isolated by scientists at the NIAID, known as VRC01, which previous work had shown neutralizes more than 90% of HIV strains. The proposed trial was to involve 3,000 African infants born to HIV-infected mothers and who are currently being breast-fed. Half the infants would receive ARV therapy plus a monthly injection of the monoclonal antibody while the other half would receive ARV therapy plus a placebo injection. Prior to the proposed study in African infants, clinical safety studies would be performed in adults and infants in the US.
The criticisms of the proposed trial appear to be threefold: 1) Antibody therapeutics are too costly for use in the developing world; 2) The lack of proven efficacy for the antibody in adults; and 3) Affordable means to prevent mother-to-child HIV transmission already exists. As an example, the Nature News article cites the work of Dr. David Ho and colleagues who found that using ARV therapy plus clean water and formula reduced the rate of mother-to-child transmission to 1%.
Counter arguments to these criticisms exist (e.g. it is not desirable to forego breast feeding due to the many positive, immune protective benefits of breast milk to infants) and an upcoming meeting in Entebbe will hopefully provide a clearer path forward that ultimately benefits the patients. In the meantime, the furor over the proposed clinical trial illustrates, yet again, the complexities and countervailing concerns that arise in driving a new therapeutic in the developing world.
© 2012-2014 Acton Biotech Consulting - See Image Credits page for attribution and license conditions for non-original images/media.
Important DISCLAIMER - This is a science & technology website and not a medical treatment or diagnostic site. No information contained within this site is a substitute for advice or direction given by qualified medical professionals, nor is it intended to inform patients regarding treatment options or disease diagnosis/prognosis. As always, individuals should consult their own medical team about issues concerning their health and well being.


