
 Listing
Listing
Human H7N9 Confirmed Cases
 Stats & Graphs
Stats & Graphs
Human H7N9 Confirmed Cases
 Latest Seasonal Flu Data from the CDC and Google
Latest Seasonal Flu Data from the CDC and Google
 Global MERS-CoV Case Count Tops 800
Global MERS-CoV Case Count Tops 800
05Jun14
The European CDC has released its Communicable Disease Threats Report for Week 22 as well as an Epidemiological Update today that shows that the rate of new human cases of MERS-CoV infection is slowing (relative to April 2014), though the global count now stands at 815 with 313 fatalities, yielding a CFR of 41%.
The following table from the ECDC report breaks down the distribution of MERS-CoV cases by country [total of 21], as of 05Jun14.
Middle East
Saudi Arabia: 689 cases / 283 deaths
United Arab Emirates: 70 cases / 9 deaths
Qatar: 7 cases / 4 deaths
Jordan: 18 cases / 5 deaths
Oman: 2 cases / 2 deaths
Kuwait: 3 cases / 1 death
Egypt: 1 case/ 0 deaths
Yemen: 1 case/ 1 death
Lebanon: 1 case / 0 deaths
Iran: 2 cases / 1 death
Europe
UK: 4 cases / 3 deaths
Germany: 2 cases / 1 death
France: 2 cases / 1 death
Italy: 1 case / 0 deaths
Greece: 1 case/ 0 deaths
Netherlands: 2 cases / 0 deaths
Africa
Tunisia: 3 cases / 1 death
Algeria: 2 cases / 1 death
Asia
Malaysia: 1 case / 1 death
Philippines: 1 case / 0 deaths
Americas
United States: 2 cases / 0 deaths
Since the update of 16May14, the geographical range of reported cases has continued to expand, with Iran and Algeria reporting their first-ever confirmed cases. In total, nearly 200 confirmed cases have been documented since the 16May14 report. However, over half of these cases were due to a retrospective update from the Ministry of Health in the Kingdom of Saudi Arabia [KSA] that encompassed 113 additional cases, including 92 fatalities, from as far back as the Spring of 2013 (see Figure. below).
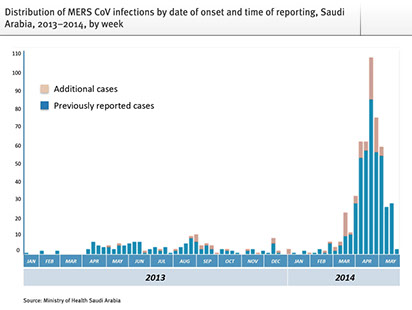
These numbers suggest that the explosive rate of new cases observed in April has slowed (see the figure, below, for a time line of reported cases globally), though the monthly rate for cases of MERS-CoV in May remains well above pre-April levels.
Distribution of confirmed cases of MERS-CoV by month of onset and time of reporting March 2012 - 1May 2014 (n=815*)

Photo Credit: European CDC
The geographical reach of the virus continues to expand with new cases in Iran amd Algeria since the last update two weeks ago.
An updated summary of the geographical spread of the virus is found in the following figure.
Distribution of confirmed MERS-CoV cases by place of reporting, March 2012 - 4 June 2014 (n=815)

Photo Credit: European CDC
Finally, as noted by the ECDC, "The source of MERS-CoV infection and the mode of transmission have not been identified, but the continued detection of cases in the Middle East indicates that there is a persistent source of infection in the region. Dromedary camels are likely an important host species for the virus, and many of the primary cases in clusters have reported direct or indirect camel exposures." A link between camels and human cases of MERS-CoV continues to strengthen as additional data accumulates, as for example in this report, citing an article just out in the New England Journal of Medicine.
 Chikungunya Outbreak in Caribbean Still Growing
Chikungunya Outbreak in Caribbean Still Growing
27May14
The latest update from the ECDC's Communicable Disease Threats Report (for Week 21) shows that the outbreak of Chikungunya in the Caribbean is still expanding, now with over 70,000 confirmed and suspected case. The table below summarizes the current outbreak in various countries in the Caribbean and South America as of 23May14, as further modified by a report today on ProMed Mail.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 20
Saint Martin 3,280 793 3
Sint Maarten 325 343
Saint Barthelemy 510 135
Guadeloupe 18,000 1,328 1
Martinique 26,670 1,515 9
French Guiana - 178
Dominica 1,578 121
Anguilla - 33
Aruba -
St. Lucia 5
St. Kitts & Nevis - 20
Saint Vincent
& Grenadines 110 57
Dominican Republic 32,519 17
Haiti 5,500 632
Antigua & Barbuda 4
Chikungunya Outbreak as of 23 May 2014

Photo Credit: European CDC
Compared to prior reports, strong upticks in cases are observed in Haiti, the Dominican Republic, Guadeloupe, and, to a lesser extent, Martinique. Imported cases (2) were reported in Panama while a false alarm was raised in Honduras. In addition, Florida reported its fourth case of imported Chikungunya.
 Chikungunya Outbreak in Caribbean Spreads to Haiti
Chikungunya Outbreak in Caribbean Spreads to Haiti
19May14
The latest update from the ECDC's Communicable Disease Threats Report for Week 20 shows that the outbreak of Chikungunya in the Caribbean is still expanding, now with over 50,000 confirmed and suspected case. The table below summarizes the current outbreak in various countries in the Caribbean and South America as of 15May14.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 20
Saint Martin 3,240 793 3
Sint Maarten - 301
Saint Barthelemy 500 135
Guadeloupe 13,000 1,328 1
Martinique 24,180 1,515 3
French Guiana - 122
Dominica 1,252 105
Anguilla - 33
Aruba - 1
St. Lucia 5
St. Kitts & Nevis - 1
Saint Vincent
& Grenadines 24 3
Dominican Republic 8,017 17
Haiti 14
Antigua & Barbuda 4
Chikungunya outbreak as of 14 May 2014

Photo Credit: European CDC
The geographical range of the virus now spans a considerable part of the Caribbean. Recent reports suggest that Chikungunya virus is spreading rapidly in Haiti with much higher numbers of suspected cases than listed even in the table, above. A spokesman for Haiti's Health Ministry is quoted a saying that some 1,529 confirmed cases have been identified, mainly from western Haiti, in the past week. This same report suggest that the Dominican Republic will soon report an additional 150-200 confirmed cases. Over the weekend, three imported cases of Chikungunya were reported in Florida. All three cases had recently traveled to the Caribbean. The same report also notes that "...there have already been as many as 100 other cases in the U.S..." Regardless, it is likely that many more cases are likely in the U.S. over the coming months.
 WHO: No MERS PHEIC & A Second U.S. MERS Case
WHO: No MERS PHEIC & A Second U.S. MERS Case
14May14
The number of new, confirmed cases of human infection by MERS-CoV continued to rise at its newly escalated rate in early May with now over 570 cases globally, including 171 deaths. In the Kingdom of Saudi Arabia, 495 cases have now been reported with 152 fatalities. Since May 1st (see previous News with Views on MERS, below), the global case count has jumped by over 150, keeping the pace observed during April of roughly 300 cases/month. However, the WHO’s latest IHR Emergency Committee Meeting on MERS has just ended without issuing a Public Health Emergency of International Concern [PHEIC]. According to a press release from the WHO, “Based on current information, the Committee indicated that the seriousness of the situation had increased in terms of public health impact, but that there is no evidence of sustained human-to-human transmission. As a result of their deliberations, the Committee concluded that the conditions for a Public Health Emergency of International Concern (PHEIC) have not yet been met. However, the Committee emphasized that its concern about the situation had significantly increased.”
The virus continues is geographical spread with a second confirmed case reported this past week in the U.S., and first-ever cases reported in Lebanon and the Netherlands. The cases in the U.S. and the Netherlands all involve individuals traveling from the Kingdom of Saudi Arabia, illustrating once again the efficiency of modern air travel in disease transmission. The CDC has updated its travel advisory to “Alert - Level 2, Practice Enhanced Precautions” but there are no restricted travel recommendations in place from either the CDC or the WHO.
Just days after the first imported case of MERS-CoV infection in the U.S. was released from an Indiana hospital, a second imported case of MERS-CoV infection in the U.S. was reported yesterday. The 44M patient is, like the first U.S. patient, a health care worker (HCW) in Saudi Arabia who flew to Florida visiting relatives late last week. He was hospitalized on 09May14 and is currently in isolation.
In addition, 20 HCWs from 2 two hospitals involved in the treatment of the 2nd confirmed U.S. patient have reportedly been placed in voluntary quarantine and two have developed respiratory symptoms. However, one of the HCWs developed symptoms only a day after treating the patient, which makes it highly unlikely the symptoms are due to MERS. The MERS-CoV virus has an incubation period typically of about 5 days. This HCW has also been placed in isolation.
Diligent precautions and careful observation remain the watch words around MERS-CoV. Consensus opinion in the public health community seems to be that the MERS-CoV remains inefficient in human-to-human transmission, especially outside of a hospital setting. However, recent sequencing data from Christian Drosten's lab clearly shows the emergence of a novel subclade of the virus in Saudi Arabia as noted and summarized on the Recombinomics website. If these genetic change can be ascribed to increased human-to-human transmission, then the MERS-CoV situation in the Middle East becomes much more concerning.
 Chikungunya Outbreak in Caribbean Spreads to Haiti
Chikungunya Outbreak in Caribbean Spreads to Haiti
14May14
The latest update from the ECDC's Communicable Disease Threats Report (as of 08May14 - Week 19) shows that the outbreak of Chikungunya in the Caribbean is still expanding, now with over 40,000 confirmed and suspected case. The table below summarizes the current outbreak in various countries in the Caribbean and South America as of 08May14.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 9
Saint Martin 3,160 793 3
Sint Maarten - 301
Saint Barthelemy 485 135
Guadeloupe 8,000 1,328 1
Martinique 19,700 1,515 2
French Guiana - 65
Dominica 1,252 105
Anguilla - 33
Aruba - 1
St. Lucia 1
St. Kitts & Nevis - 1
Saint Vincent
& Grenadines 24 3
Dominican Republic 7,520 17
Haiti 14
Antigua & Barbuda 1
The geographical range of the virus now spans a considerable part of the Caribbean with new cases in Haiti and Antigua & Barbuda. A recent article in the Washington Post highlights concerns over the spreading wave of Chikungunya cases with Caribbean health officials waring that "that they “cannot stop” a rapidly spreading mosquito-borne virus..."
 MERS-CoV Case Count Explodes
MERS-CoV Case Count Explodes
01May14 Updated 02May14
The European CDC reports, in the latest Epidemiological Update on MERS that, as of 30 April 2014, 424 cases of human infection by MERS-CoV have been reported globally, including 131 deaths. A Communicable Disease Threat update of 02May14 has added more cases, bringing the global total to 450. All cases have either occurred in the Middle East or have direct links to a primary case infected in the Middle East.
The following table from the ECDC report breaks down the distribution of MERS-CoV cases by country.
Middle East
Saudi Arabia: 368 cases / 107 deaths
United Arab Emirates: 49 cases / 9 deaths
Qatar: 7 cases / 4 deaths
Jordan: 5 cases / 3 deaths
Oman: 2 cases / 2 deaths
Kuwait: 3 cases / 1 death
Egypt: 1 case/ 0 deaths
Europe
UK: 4 cases / 3 deaths
Germany: 2 cases / 1 death
France: 2 cases / 1 death
Italy: 1 case / 0 deaths
Greece: 1 case/ 0 deaths
Africa
Tunisia: 3 cases / 1 death
Asia
Malaysia: 1 case / 1 death
Philippines: 1 case / 0 deaths
Since the update of 22Apr14, the geographical range of reported cases has continued to expand, with both Egypt and Greece reporting their first-ever confirmed cases. More importantly, the number of reported cases in April (243) exceeded the sum total of all previous cases since 2012 (207), providing an unmistakable landmark of an emerging viral disease breaking out (see the figure, below, for a time line of reported cases globally).
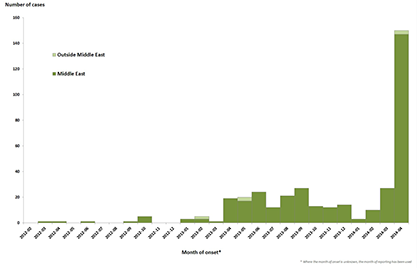
Photo Credit: European CDC
Even this figure is slightly misleading as to the extent of the surge in MERS cases - an additional 50 cases were reported in April subsequent to the closing date of data for this figure. The April surge in MERS-CoV cases is best seen in the following figure from the ECDC Epidemiological Update.
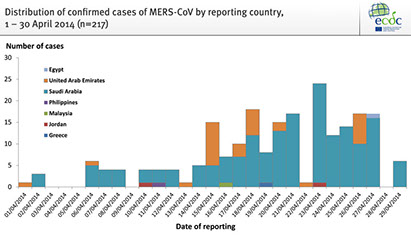
Photo Credit: European CDC
Note that the majority of the reported cases occurred in the second half of the month. An updated summary of the geographical spread of the virus is found in the following figure.
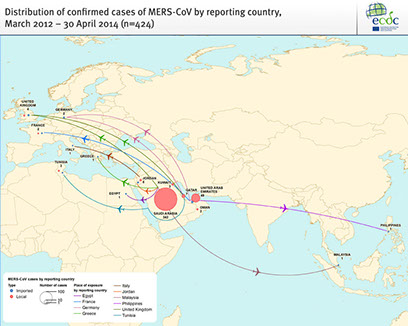
Photo Credit: European CDC
Several attributes of this surge are worthy of note. First, 62 of the 243 cases reported in April occurred in health care workers (HCWs). This is roughly double the rate of HCW infection from the total infection pool observed from 2012-March 2014. Second, the vast majority of the 243 cases reported in April occurred in either the Kingdom of Saudi Arabia (KSA; 179 cases) or the United Arab emirates (32). Indeed, the surge in these countries continues with an additional 26 cases reported in the KSA today.
Finally, the season for this sudden surge in MERS cases is not clear. A large number of April cases in the KSA were found in a few locales, especially the city of Jeddah. A recent report to ProMed has detailed nearly complete genomic sequencing of three clinical isolates of MERS-CoV from early in the month (including 2 from Jeddah) showed that "Genome sequences of all 3 viruses are highly similar to each other but not identical, and are highly similar to a large number of known MERS-CoV sequences (consult http://www.virology-bonn.de for a phylogeny; genome overview in Cotten 2014). There are no genome insertions or deletions suggestive of sudden major changes. The receptor-binding domain in the spike protein thought to influence the virus's ability to be transmitted or spread is 100 percent identical to the binding site in a large number of known MERS-CoV genome sequences. Based on genome comparison with other MERS-CoV strains there is no reason to assume that the sequenced viruses from Jeddah have acquired changes increasing their pandemic potential." That said, Recombinomics has pointed out that this analysis places the 3 examined genomes in their own sub-clade with the three isolates possessing "... 11 polymorphisms (listed below) which were present in all three sequences from the Jeddah cases, and were not present in any public MERS sequence. Thus, the 11 markers define the novel MERS sub-clade and raise concerns that one or more of these changes is responsible for the dramatic spike in MERS cases, which have led to at least five exported cases from Jeddah ( to Jordan twice, Malaysia, Greece, and UAE)." Additional sequencing, especially of isolates obtained later in the month, will clarify the situation. And of course, factors other than changes to the viral genome could account for the dramatic surge in MERS-CoV cases (e.g. a change in infection control procedures at local hospitals), but little evidence is currently available to support any these other possibilities.
In the meantime, the crucial role of camels as a zoonotic reservoir for MERS-CoV continues to evolve. Whole genome analysis of nasal swabs taken from camels in KSA was recently reported and showed that "Consensus dromedary MERS-CoV genome sequences were ... identical to published human MERS-CoV sequences." However, the precise relevance to human infection is not yet clear. " However, in contrast to individual human cases, where only clonal genomic sequences are reported, detailed population analyses revealed the presence of more than one genomic variant in individual dromedaries. If humans are truly infected only with clonal virus populations, we must entertain a model for interspecies transmission of MERS-CoV wherein only specific genotypes are capable of passing bottleneck selection."
Careful inspection of the monthly case totals since 2012 does show that in 2013 a drop in case counts occurred in March followed by an uptick in cases in April that persisted (more or less) at the new higher level for the rest of the year. The same phenomenon was observed in January and April of this year, though with a much greater amplitude to the April uptick. It will be of interest to see if the number of cases continues to climb and then recede or if, like last year, we persist with roughly 200 or so new MERS-CoV cases every month till next Spring.
 West African Ebola Outbreak Due to Novel Strain of Virus
West African Ebola Outbreak Due to Novel Strain of Virus
17Apr14
An important new report just published online at The New England Journal of Medicine provides preliminary insight into the outbreak of Ebola Virus Diesease [EVD] in Western Africa, including initial virologic and genomic data. Of greatest potential interest is the finding that the current outbreak is ascribable to a new “sister” of the Zaire (EBOV) strain of Ebola virus. Specifically, total sequencing of the viral genome was performed on isolates from three patients. The three viral genomic sequences were almost identical to each other (6 positions of nucleotide differences, four of which are synonymous) and “showed 97% identity to EBOV strains from the Democratic Republic of Congo and Gabon. Phylogenetic analysis of the full-length sequences by means of Bayesian and maximum-likelihood methods revealed a separate, basal position of the Guinean EBOV within the EBOV clade…” This and other data “….suggests that the EBOV strain from Guinea has evolved in parallel with the strains from the Democratic Republic of Congo and Gabon from a recent ancestor and has not been introduced from the latter countries into Guinea.”
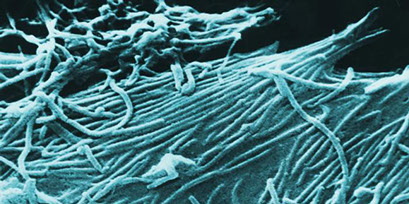
Ebola Virions; Image Source: CDC
Another feature of note in this report is an initial back-looking epidemiological investigation that identified an index case as a 2F patient from Meliandou in Guéckédou prefecture who died in early December of 2013. Subsequent spread of the virus to nearby towns (by February of 2014) was facilitated by a health care worker from Guéckédou. An initial set of 13 confirmed cases can be linked to four regionally proximal clusters and a transmission train that “…started in the prefecture Guéckédou and then spread to Macenta and Kissidougou…”
Overall, the study concludes that the available data suggests “…a single introduction of the virus into the human population. This introduction seems to have happened in early December 2013 or even before.” Phylogenetic analysis is congruent with this epidemiological assessment, establishing a Guinean strain of EBOV that “…evolved in parallel with the strains from the Democratic Republic of Congo and Gabon from a recent ancestor and has not been introduced from the latter countries into Guinea.” How long the precursor strain was present before a human infection occurred is unknown, as is the precise zoonotic reservoir for the virus.
 Chikungunya Outbreak In Caribbean Tops 25,000; New Outbreak in Tonga
Chikungunya Outbreak In Caribbean Tops 25,000; New Outbreak in Tonga
16Apr14
The outbreak of chikungunya virus in the Caribbean continues. According to the latest Communicable Disease Threats Report (for Week 15, as of 28Mar14) from the European CDC, there have been more than 25,000 probable and confirmed cases in the region, including six fatalities. The table below summarizes the current outbreak in various countries in the Caribbean.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 7
Saint Martin- 2,910 791 3
Sint Maarten - 224
Saint Barthelemy - 444 135
Guadeloupe - 3,690 942 1
Martinique - 13,500 1,284 2
French Guiana - 42
Dominica 764 81
Anguilla - 14
Aruba - 1
St. Kitts & Nevis - 1
Saint Lucia 1
Dominican Republic 767*
Adding to the potential concern about the further spread of the virus in the Americas, investigators from Brazil and France published a study last week in the J. of Virology that both of the two known mosquito vector species "...were capable to transmit all three CHIKV genotypes, and TE [transmission efficiency] reached alarming rates as high as 83.3% and 96.7% in Ae. aegypti and Ae. albopictus populations, respectively. These results suggest that the barrier for spread of the virus through the Americas will be low and resulted in media stories about an impending catastrophic epidemic that could even affect the World Cup next year in Brazil.
At the same time, the Australia News Network is reporting the first-ever outbreak of chikungunya in the pacific island state of Tonga. As many as 10,000 people may be affected, almost 10% of the island's population.
 MERS-CoV Case Count Now Over 220
MERS-CoV Case Count Now Over 220
14Apr14
The European CDC is reporting in its Week 15 Communicable Disease Threats Report that the global number of laboratory-confirmed human cases of SARS-like MERS corona virus infection now stands at 229 with 91 fatalities. The Kingdom of Saudi Arabia continues to be the hardest hit with 182 laboratory-confirmed cases and 67 fatalities. Over the past week, considerable alarm and anxiety gripped the Kingdom as a cluster of cases emerged in Jeddah affecting health care providers, part of an overall surge in cases this past two weeks (see here). In parallel, the UAE recently announced an outbreak of 6 MERS-CoV cases among paramedics. These events, taken together, raise questions about infection control in the Mideast since the MERS-CoV virus is not highly transmissible between humans.
The following table from the ECDC report breaks down the distribution of MERS-CoV cases by country.
Saudi Arabia: 182 cases / 67 deaths
United Arab Emirates: 19 cases / 8 deaths
Qatar: 7 cases / 4 deaths
Jordan: 4 cases / 3 deaths
Oman: 2 cases / 2 deaths
Kuwait: 3 cases / 1 death
UK: 4 cases / 3 deaths
Germany: 2 cases / 1 death
France: 2 cases / 1 death
Italy: 1 case / 0 death
Tunisia: 3 cases / 1 death
And now, another country, Yemen, has reported its first case of human MERS-CoV infection. The rate of new cases appears to be increasing as we head into Q2 for 2014, as shown in the summary slide below from the ECDC report.
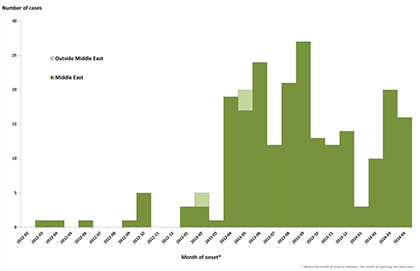
Photo Credit: European CDC
While there have been instances of local transmission among patients, for example in France and the UK, the risk of secondary transmission remains low. More generally, person-to-person transmission has been noted among close contacts and health care providers (about 50 of the 229 confirmed cases). However as noted in the prior ECDC report, the extent of secondary transmission has been limited. Of course the single largest issue looming over this outbreak is that the source and mode of transmission have yet to be identified, though recent work is currently pointing towards a potential role for camels in the etiology of the disease.
 W. African Ebola Virus Out-break Death Toll Climbs to 111
W. African Ebola Virus Out-break Death Toll Climbs to 111
11Apr14 Updated 13Apr14
The latest data from the WHO, in a report dated 10Apr14, shows that a total of 158 clinically compatible cases of Ebola virus disease (EVD) in the west African nation of Guinea, including 101 deaths have been officially reported. A total of 6 districts of Guinea have reported cases including Conakry, with 20 confirmed patients. "A total of 66 clinical cases have been laboratory confirmed (42%), while 87 of the remaining clinical cases are classified as probable cases and 4 as suspected cases. Twenty-four of the 101 deaths have been laboratory confirmed."
In addition to the situation in Guinea, Liberia has reported a cumulative total of 5 laboratory confirmed cases and 20 suspected cases of EVD. Mali has reported a total of 6 suspected cases of EVD, though no confirmed cases. And countries such as Sierra Leone and the Ivory Coast remain on high alert.
The essential feature that makes this particular outbreak of EVD so noteworthy was elegantly summarized in a piece for The Independent by Michel Van Herp, an epidemiologist with Médecins Sans Frontières. "I've worked in every major outbreak of ebola since 2000. What makes this one different is its geographical spread, which is unprecedented."
As noted previously (see below), an outbreak of EVD in western Africa is also unprecedented. In a report today from Bloomberg News, the various socio-economic consequences of and EVD outbreak in this part of Africa are summarized. And, an additional 10 fatalities were reported.
These unusual characteristics will mean that this EVD outbreak is both worrisome and challenging for global health care agencies.
 Confirmed Case Count of Human H7N9 Infections Hits 400
Confirmed Case Count of Human H7N9 Infections Hits 400
24Mar14
The global number of confirmed human cases of H7N9 influenza infection has now hit 400 with the report today from Xinhua of another case in China’s Guangdong province. In the past month, the global reach of H7N9 has continued to spread with first-ever cases in Malaysia and the Chinese province of Jilin. Some 264 of these cases and at least 72 fatalities have occurred in the current flu season (starting last fall), roughly 252 since the start of 2014. The number of new human cases has declined over recent weeks from the highs seen in late January, offering hope that this season’s peak may have already passed. As noted in the Xinhua article, only 12 H7N9 cases were reported so far in March for Guangdong Province, China's hardest hit province this season and down from the 39 reported in February. The closure of live poultry markets in major Chinese cities, as last Spring, may be responsible for the dramatic fall off in reported cases. More detailed information on the H7N9 cases can be found here and here.
Recombinomics recently evaluated sequence data from the recent 5 month old infant diagnosed with H7N9 influenza
In Hong Kong (traveling from Guangdong Province). The infant was last reportedly in stable condition. Inspection of the sequence data illuminated the following points:
1. The HA of the clinical isolate included the mammalian adaptation marker Q226L.
2. The PB2 sequence did NOT show the typical E627K mammalian adaptation marker, retaining the avian sequon. (Just this past week, a new paper came out in the Journal of General Virology which demonstrates “…that the PB2 E627K mutation, which occurs in over 70 % of the H7N9 patient isolates, promotes the replication of H7N9 virus by enhancing PB2 polymerase activity and enhances virulence in mice.”)
3. The sequence of the PA gene from the infant’s isolate did NOT have the mammalian adaptation marker L336M (common in isolates from southern China) and was more closely related to PA sequences in isolates from northern China.
The upshot of this analysis is “…that milder H7N9 without these adaptation may be widespread, and largely missed due to surveillance efforts focused on more severe cases.” H7N9 influenza has been difficult to monitor and to ascribe a source of infection in part because the disease is so mild in birds. The prospect of a comparable set of human infections could greatly complicate surveillance and containment and potentially raise the risk of new reassortants. These concerns take on added weight if one considers the recent (3/17) article in The Lancet Respiratory Medicine which concludes that “Seasonal influenza and the 2009 pandemic strain were characterised by similar high rates of mainly asymptomatic infection with most symptomatic cases self-managing without medical consultation. In the community the 2009 pandemic strain caused milder symptoms than seasonal H3N2.” How such a large population of subclinical cases (about 75% of all infections) of influenza (for any strain) impacts transmission is an important, unanswered question.
 Dengue Outbreak in Oceania, High activity in the Americas
Dengue Outbreak in Oceania, High activity in the Americas
24Mar14
The outbreak of dengue continues unabated in Fiji with nearly 12,000 cases and 12 deaths reported since last October, according to the latest CDT report from the European CDC. The outbreak in Fiji is especially difficult since it is largely DEN-3 instead of the more typical (for Fiji) DEN-1 strain; DEN-3 has never been seen before in Fiji. Dengue has also been a serious problem in Malaysia so far this year, with over 12,000 cases reported, a 4-fold increase over the same period last year. In Singapore, over 3,500 cases have been reported this year.
The CDT report also notes high levels of dengue activity in Mexico and Central America. Over 1,900 cases of dengue have been reported in Mexico this year while Guatemala has reported 845 cases and two deaths. In contrast, the dengue epidemic in Brazil has dropped 80% in the first two months of 2014 with 87,000 notified cases (as compared to the same period last year with 427,000 cases). Similarly, Costa Rica has reported 1,262 cases through mid-February, a 64% decrease over the same period last year. In the meantime, Peru has declared a state of emergency as 93 cases of dengue have been reported in the provinces of La Convención and Piura.
A summary of global dengue activity so far this year is shown in green in the map, below.

Photo Credit: WHO Interactive Map
 The 7th and 8th Human H5N1 Cases Reported in Cambodia
The 7th and 8th Human H5N1 Cases Reported in Cambodia
13Mar14
The seventh and eighth confirmed human cases of H5N1 infection in Cambodia this year have been announced in a joint press release from the Ministry of Health of the Kingdom of Cambodia, and the World Health Organization. One of the patients (8M) is reportedly recovering while the other patient (11M) has died. Of the eight cases this year in Cambodia, three (7M, 3M, and 11M) have proven fatal. Almost all of the confirmed cases this year involve direct human exposure to birds (dead or alive) infected with H5N1.
In a related news story, government officials in Cambodia are reporting that "The border provinces of Takeo and Kampong Cham have been witness to the highest number of H5N1 poultry outbreaks since the disease was first discovered in early 2004". Border control of infected birds is critical since Vietnam is wrestling with the spread of a novel H5N1 clade, clade 2.3.2.1C, across the country.
 A U.S. Flare-up in Measles, a Global Killer of Children
A U.S. Flare-up in Measles, a Global Killer of Children
12Mar14
There has been a burst of recent measles cases in the US, serving as a reminder that this still deadly killer of children around the globe requires our constant attention, even here. A recent online article at Al Jazerra America puts the recent tally at 53 cases (citing CDC data) but more recent reports of other outbreaks (see here and here, for example) have already pushed the tally higher. Recent cases have also been reported in Canada (see here, here, and here). For an excellent ongoing overview of recent cases and their context, please see Dr. Vincent Iannelli’s online article.
Measles (a.k.a. rubeola) is a highly contagious viral disease spread by close personal contact via respiratory droplets or direct contact with secretions. Humans are the only natural reservoir for the virus. Most notable for its well-known rash, measles is also characterized by the 4D+3C shorthand: 4 Days of fever (that can exceed 104 °F) plus Cough, Conjunctivitis, and Coryza [common cold]. As noted by the CDC, “About one out of 10 children with measles also gets an ear infection, and up to one out of 20 gets pneumonia. For every 1,000 children who get measles, one or two will die.” This contrasts to the situation in the U.S in 1912 where, for every 1,000 children who got the measles, 25 died.
Complications from measles are often the real clinical problem and actually presents greater risks for adults than children. Where malnutrition and poor health care are present, as in the developing world, mortality rates can reach as high as 34% [reference], principally due to “…a young age at infection, crowding, underlying immune deficiency disorders, vitamin A deficiency, and lack of access to medical care.”
In a recent MMWR article on global efforts to eradicate measles, the authors note that global vaccination efforts over the period 2000-2012 reduced the global case count of measles from “…853,480 to a historic low of 226,722, and measles incidence decreased 77%, from 146 to 33 cases per million population per year…” and that during this same period, deaths due to measles “…decreased 78%, from 562,400 to 122,000”. These are stunning and wonderful results, saving nearly 14M lives over the cited 13 year period. Indeed, the U.S. declared measles eliminated in 2000 since there were no longer periods of continuous transmission lasting greater than 12 months (a transmission event is a chain of transmission involving 3 or more confirmed cases). The last reported measles death in the U.S. was in 2003.
But this progress has, in turn, illuminated a new problem: the path to global eradication is confounded by an emerging risk of new infections even in developed, well-vaccinated populations. As seen in the graph, below, measles cases in the U.S. have been trending up over the past 6 years with essentially all of the cases occurring in unvaccinated/under-vaccinated populations “seeded” with an imported case. Thus, U.S. cases occur as local outbreaks sparked by an imported case and transmitted to others in a susceptible local population.

The root of the problem is two-fold. First, the global battle to eradicate measles has had its ups and downs. As noted in the MMWR article cited above, the global case count has not declined smoothly; “The decrease in 2012 occurred in all regions and followed 3 years of increasing numbers of cases.” Indeed, measles appears to be especially problematic.
As noted in Feb. of this year by the International Business Times, “Looking at vaccine-preventable disease outbreaks in the first month of the year offers a good snapshot – before the global map of outbreaks gets crowded. In January, 24 outbreaks of measles were reported, some on every continent, afflicting at least 336 individuals, according to data compiled here by the Council on Foreign Relations. Showing just how persistent the measles paramyxovirus is: last month it was almost the only vaccine-preventable infection to show up on the global radar. The only other vaccine-preventable infection to appear in global media reports last month was polio in war-torn Pakistan and Afghanistan. No mumps. No rubella. No whooping cough. But measles popped up worldwide.” Even today, inspection of the map shows mainly measles outbreaks with only the addition of polio in Pakistan and Afghanistan plus whooping cough in the U.S.
The second root of the problem is the relative ease with which import cases, seeded by travel to/from external outbreak or measles-endemic regions can take hold in local populations. These susceptible local populations seem to be growing, though there are no hard numbers available. As noted in the Al Jazeera America article, “The resistance to getting inoculations comes from an unlikely variety of views: Deeply conservative parents reject the government’s interfering with their child rearing; orthodox religious groups dislike vaccines for being man-made, not God-given; and well-educated, health-conscious, affluent and Internet-literate parents don’t see vaccines as organic or natural.” Regardless of reason, the susceptible population doesn’t only effect their constitutive members: infants who have yet to receive their first vaccination (typically infants less that 1 year of age) are susceptible to measles infection.
Clearly there is a need to encourage everyone to get the recommended set of vaccinations in a timely manner. But resistance seems, oddly, entrenched and growing. Much of this resistance is rooted in the now debunked putative connection between autism and vaccines. But as noted in a 2011 article from Vaccine News Daily, “It's very easy in our media-driven, easy-access-to-information society to scare people," Dr. Tanya Remer Altmann, a spokeswoman for the American Academy of Pediatrics, said, according to USA Today. "It's much more difficult to unscare them."
 Confirmation: Aggressive Tx Clears HIV Infection in Newborns
Confirmation: Aggressive Tx Clears HIV Infection in Newborns
06Mar14
Results presented yesterday at the Conference on Retroviruses and Opportunistic Infections in Boston confirm earlier results that aggressive treatment of HIV-infected newborns can "dramatically restrict -- and perhaps eliminate -- infection", according to a MedPage Today news report. The report covers the remarks of Dr. Deborah Persaud (Johns Hopkins) regarding a second infant who received triple agent anti-retroviral therapy within hours of birth.
This second case, arising from Los Angeles County, showed that "...within days, almost all signs of HIV had disappeared. The plasma viral load, for instance, was and has remained undetectable, defined as fewer than 20 copies per milliliter."
Further, there is "...no indication that the child harbors a reservoir of "replication-competent virus" even if fragments of HIV RNA or DNA are present."
The original case, the so-called Mississippi baby, stopped receiving anti-viral therapy early and inadvertantly. Nevertheless, the infant is now 41 months old and remains free of HIV. The California baby remains on therapy so it is not possible to conclude that the virus has been eliminated permanently.
With this confirmation in a second infant, the idea that very early and aggressive treatment of neonates with anti-HIV regimens can severely restrict the virus, to the point of being undetectable, is now on more solid footing. According to the report, "Persaud added that plans are underway for a prospective international clinical trial involving 54 infants who will be treated at birth or very soon after, with planned treatment interruptions at age 2." The results of such a trial will be eagerly anticipated since they offer the hope of dramatically altering the lives of infected babies born to HIV-infected mothers.
 Cambodia Confirms Fourth and Fifth Human H5N1 Cases
Cambodia Confirms Fourth and Fifth Human H5N1 Cases
04Mar14
The number of laboratory-confirmed cases of human H5N1 infection this year in Cambodia has increased to six with confirmation by the Ministry of Health for the Kingdom of Cambodia in a press release. The two patients (10F and 11F) were from the same province, were exposed to dead poultry, and have both now recovered.
These cases brings the total number of confirmed H5N1 cases in Cambodia since 2005 to 52. All but 18 of the patients died due to infection. The vast majority of the cases (40) occurred in children under 14.
 Chikungunya Outbreak Keeps Growing in Carribean
Chikungunya Outbreak Keeps Growing in Carribean
25Feb14 Updated 02Mar14
The first-ever outbreak of chikungunya virus infections in humans in the Caribbean continues to grow. According to the most recent update from the ECDC, the number of suspected cases has grown from about 1000 a little over a month ago to over 5900 suspected cases as of 21Feb14. As of 28Feb14:
Suspected Cases Confirmed Cases
Saint Martin- 2,030 765
Sint Maarten - 115
Saint Barthelemy - 380 127
Guadeloupe - 1,460 476
Martinique - 3,940 1,058
Br. Virgin Islands - 6
Dominica - 45
Anguilla - 11
Aruba - 1
St. Kitts & Nevis - 1
In addition, the same update notes the first confirmed/suspected cases (17) of chikungunya infection in South America (French Guiana). By the end of February, the ECDC's Communicable Disease Threats Report for Week 9 [23Feb-01Mar14] cited nearly 8000 suspected cases with three fatalities.
Concerns about a possible spread to North America may have been already realized given a recent ProMed mail on three suspected cases of Chikungunya in the Yucatan.
 New Human H5N1 Fatalities in Cambodia & Vietnam
New Human H5N1 Fatalities in Cambodia & Vietnam
22Feb14
The third confirmed case of human infection by H5N1 influenza this year in Cambodia has been reported. The patient (4M) is reportedly in good condition. This follows closely reports earlier this month of two siblings (7M & 3F) who contracted H5N1 on Feb 1st and died on Feb. 10th, as well as an earlier 5M patient who reportedly recovered. Cambodia has now reported an aggregate total of 51 cases of human H5N1 infection, 34 of which were fatal. Over half of these cases (26) occurred last year including 19 fatalities.
In January, two fatal human cases of H5N1 infection (60F & 52M) were reported in Vietnam. These human cases have occurred against a backdrop of a massive outbreak of H5N1 in Vietnamese poultry, now reportedly covering outbreaks in eight provinces and the culling of over 30,000 birds.
 U.S. Flu Activity in Week 5: High But Slowly Ebbing
U.S. Flu Activity in Week 5: High But Slowly Ebbing
07Feb14
The latest data from the CDC for the week ending February 1st (week 5) has been published. The data shows that flu activity in the U.S. again is still robust, though most indicators were once again down slightly from the week prior (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza fell again to 19.6% nationally, compared to 21.1% the prior week and 23.1% the week before. All regions had percent flu positive values in excess of the national rate, save Regions 6 [AR, LA, NM, OK, TX], 7 [IA, KS, MO, NE], and 8 [CO, MT, ND, SD, UT, WY] at 19.3%,19.4% and 17.9% respectively. The following graph illustrates the overall trends by region for % flu positive samples this season.
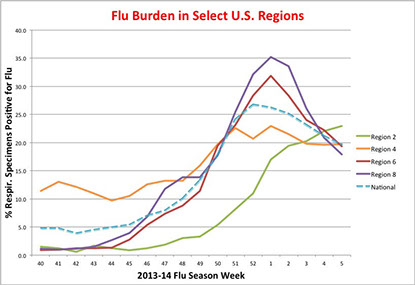
The pneumonia and influenza (P&I) mortality index is 8.6% (8.8% last week), above the epidemic threshold of 7.3% for Week 5. There were three influenza-associated pediatric deaths reported, all ascribed to not-subtyped influenza A. Nine influenza-associated pediatric deaths were reported last week. A total of 40 influenza-associated pediatric deaths have been reported this season.
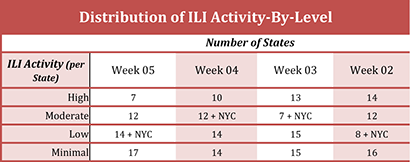
The proportion of outpatient visits ascribed to influenza (ILI) was 3.2% (versus 3.3% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows seven states with “high ILI activity” (see table below) and twelve states with "moderate ILI activity". When typed, the majority of isolates were influenza A (~93% of typed specimens) and, while only 56% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 96%; 4% were H3N2).
The number of Tamiflu-resistant isolates detected this season increased to 23, and the % of tested isolates found to be Tamiflu-resistant increased to 0.8% (from 0.9%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
With leading indicators down for a fourth week in a row, there is an increasing likelihood that the influenza season may have already peaked for the season, though the nation still remains firmly in the grip of an active season. And given the atypical patient demographic (most hospitalization are in those aged 18-64), the ebbing tide of influenza will continue as a "high impact" virus this season.
 Confirmed Cases of H7N9 Jump to 205, at Pace With Last Spring's Peak Rate
Confirmed Cases of H7N9 Jump to 205, at Pace With Last Spring's Peak Rate
19Jan14
The global number of confirmed cases of human infection by influenza H7N9 has swollen to 205 with 54 fatalities. Nine new cases were reported in Zhejiang Province, three each in Fujian and Guangdong Provinces, and an additional case was reported in Shanghai. The latest stats and a breakdown of new cases by country & province can be found here. A table with details of confirmed H7N9 cases can be found here.
Perhaps because of the sudden upward spike in confirmed H7N9 cases in China since the start of 2014, ProMED Mail is has published a notice from Hong Kong's Information Services Department stating that "Starting from 24 Jan 2014, Hong Kong and the Mainland will conduct serological testing for H7 avian influenza (AI) on live poultry at Mainland registered farms and the Man Kam To Animal Inspection Station. Serological testing will also be introduced to local poultry farms in Hong Kong on the same day."
While the city of Shanghai has previously announced that live poultry trading will be suspended from 31Jan14 till 30Apr14 to control the H7N9 virus, this newest step represents a considerable escalation of control efforts in Hong Kong and the mainland. the rationale behind these moves is simple, as re-iterated in the ProMED Mail posting: ""The traditional Chinese New Year holiday period is approaching with its associated large-scale population movement and enhanced slaughter and consumption of poultry, which the local and national authorities will have difficulty controlling. During this period there will be enhanced opportunity for the evolution of H7N9 virus with potential for transition from person-to-person."" such market intervention seemed to pay dividends last spring and hopefully shall again.
 Chikungunya Outbreak Grows in Carribean
Chikungunya Outbreak Grows in Carribean
19Jan14
The first-ever outbreak of chikungunya virus infections in humans in the Caribbean continues to grow. A new posting on ProMED Mail updates the tally of confirmed & suspected cases in the Caribbean as of 17Jan14:
Suspected Cases Confirmed Cases
Saint Martin- 490 294
Saint Barthelemy - 81 312
Guadeloupe - 76 27
Martinique - 340 127
In addition, the same posting noted the first confirmed case of chikungunya infection in the Commonwealth of Dominica.
The CDC has issued a HAN advisory as well as a notice to travelers on Dec. 13th. Given the identity of the mosquito vectors employed by the virus (Aedes aegypti and A. albopictus), there is a real concern for eventual cases on the U.S. mainland, such as was observed for another, related viruses - dengue fever virus and West Nile virus.
 Caribbean Chikungunya Cases Now Top 100,000
Caribbean Chikungunya Cases Now Top 100,000
05Jun14
Three recent publications [ one from the CDC in a MMWR report issued today, another from the ECDC in the Week 22 edition of the Communicable Disease Threats Report (though 02Jun14), and finally a ECDC Epidemiological Update published today ] all highlight a doubling in the number of cases of Chikungunya in the Caribbean over the past 14 days, to now over 100,000 suspected and confirmed cases with at least 14 deaths.
As noted in the MMWR article, “As of May 30, 2014, a total of 103,018 suspected and 4,406 laboratory-confirmed Chikungunya cases had been reported from these areas.* The number of reported cases nearly doubled during the previous 2 weeks. More than 95% of the cases have been reported from five jurisdictions: Dominican Republic (38,656 cases), Martinique (30,715), Guadeloupe (24,428), Haiti (6,318), and Saint Martin (4,113). The highest incidences have been reported from Saint Martin (115 cases per 1,000 population), Martinique (76 per 1,000), Saint Barthelemy (74 per 1,000), and Guadeloupe (52 per 1,000). ” The table below summarizes the current outbreak in various countries in the Caribbean.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 20
Saint Martin 3,280 793 3
Sint Maarten 325 301
Saint Barthelemy 520 135
Guadeloupe 24,428 1,328 1
Martinique 30,715 1,515 9
French Guiana - 222
Dominica 1,817 122
Anguilla - 33
Aruba - 1
St. Lucia 5
St. Kitts & Nevis - 21
Saint Vincent
& Grenadines 110 57
Dominican Republic 38,656 17
Haiti 6,318 632
Antigua & Barbuda 4
Puerto Rico 1
Rep. of Guyana 12
Media reports indicate that the frenzied expansion in cases of Chikungunya is outstripping numbers reported by the WHO, CDC, or the ECDC. For example, one report published today states that “In the Dominican Republic alone, for example, the health ministry says it has detected more than 103,000 cases.”
Chikungunya has also extended its geographical reach over the past two weeks with the first confirmed case in San Juan, Puerto Rico, and the first locally-infected cases in the Co-operative Republic of Guyana, the latter becoming the 2nd country in South America with local transmission. And CIDRAP News reported on 02Jun14 that Chile and Barbados are investigating their first imported cases. The tally of imported cases in the U.S. has now risen to 30 according to a media report issued today.
As noted in the Communicable Disease Threats Report (Week 22, thru 02Jun14), there have been media reports of imported cases in Panama (ex Haiti and the Dominican Republic), Venezuela (ex the Dominican Republic), as well as an imported case in the Pacific island of Tahiti in French Polynesia (ex Guadaloupe).
Chikungunya Outbreak as of 23 May 2014

Photo Credit: European CDC
 West African Ebola Outbreak: Case Count Now Exceeds 300
West African Ebola Outbreak: Case Count Now Exceeds 300
05Jun14
The WHO has issued an update on the Western Africa Ebola virus outbreak on 04Jun14 and a Communicable Disease Threat update for Week 22 that report a spike in cases with an additional 37 new clinical cases of Ebola virus disease [EVD] and 21 fatalities in Guinea, 13 new cases in Sierra Leone (3 confirmed and 10 suspected), and one new suspected case in Liberia, all since 28May14.
The new cases in Guinea were localized largely in Telimele and Gueckedou (30/37 cases and 18/21 fatalities) with other cases in Conakry and Macenta. Most of the new cases (12/13) in Sierra Leone were from Kailahun. The suspected case in Liberia was an individual from nearby Kailahun who died in Liberia and was taken back to Kailahun for burial.
Ebola Virions; Image Source: CDC
These new cases bring the cumulative number of cases in Guinea to 328 (193 lab confirmed, 80 probable, and 55 suspected) of which 208 were fatal. The cumulative number of cases in Sierra Leone is now 79 (18 confirmed, 3 probable, and 58 suspected) including 6 deaths (five of which occurred in the past 10 days). There have been no new cases of EVD in Liberia since 09Apr14 and the cumulative total still stands at 27 cases and now 14 deaths.
The current outbreak of EVD in Western Africa is now approaching the deadliest outbreak ever of EVD, that in Democratic Republic of Congo in 1976 that killed 280. Doctors Without Borders is reportedly concerned about the "resurging" EVD outbreak, especially as regards its vast geographical spread. The relative lack of communication and infrastructure in this region could yet facilitate a wider outbreak of EVD.
 Pertussis Spreads Its Wings in California
Pertussis Spreads Its Wings in California
04Jun14
A new posting on ProMed Mail details the continuing spread of pertussis in California where, for example, "...the number of whooping cough cases in Sacramento County so far in 2014 nearly doubling what the county confirmed for the entire year in 2013. Among 3 other counties in the capital region, only Yolo County is seeing a similarly dramatic increase, though the number of cases confirmed there is far lower." Media reports also indicate increasing spread within the state, for example in Marin County where local media have reported "near epidemic" levels.
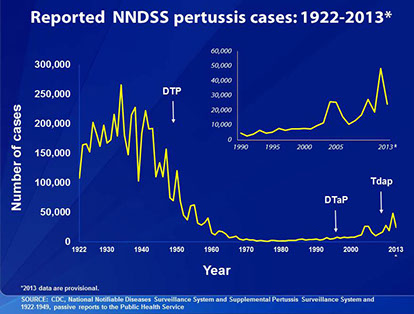
According to cited figures from the California Department of Health, there have been 2649 cases of pertussis this year to date and two pediatric fatalities. Nor is California alone in seeing rising concerns about pertussis outbreaks. Earlier this year, local outbreaks were reported in Texas, Ohio, Utah (link) and Arkansas (link), Colorado (link), and South Dakota (link). All told, there have been nearly 10,000 cases reported so far this year in the U.S. In 2013, roughly 24,000 cases were reported in the U.S. The graph. below, illustrates the historical incidence of whooping cough in the U.S. including recent trends upward.
It is likely that the culprit behind this outbreak of pertussis is the waning immunity conferred by the use of the acellular pertussis component of the current DTaP [Diptheria, Tetanus, acellular Pertussis] vaccine. This waning immunity in the pediatric/teen population creates a reservoir for Bordetella pertussis that places infants, especially those less than 6 months of age, at risk. We have discussed this issue at length previously on these pages (please see the Archives).
Another contributing factor to these outbreaks could also be reductions in the levels of vaccination. As reported in an online article on Examinar.com, the top five states reporting pertussis cases this year all allow parents to opt-out of required vaccinations for their school-age children. In Texas, a total of 30,000 such exemptions have been granted according to one news report.
A third possibility for the recent spike in cases is that the pathogen has changed and the current vaccine is no longer effective against the new form of the bacterium. An example of such a change is the report last year of pertactin-negative strains of pertussis in the U.S. (please see this web page at the CDC for a discussion). Pertactin is an important, but by no means sole, component against pertussis in the current DTaP vaccine.
Regardless of which of these factors or combination of factors lies behind the recent up-tick in pertussis, re-doubling our efforts to keep this deadly killer of young infants at bay is clearly an important societal priority.
 Third U.S.MERS-CoV Case; Global Count Still Climbing
Third U.S.MERS-CoV Case; Global Count Still Climbing
19May14
The European CDC has released its Communicable Disease Threats Report for Week 20 and denotes 621 laboratory-confirmed cases of human infection by MERS-CoV, including 188 deaths.
The following table from the ECDC report breaks down the distribution of MERS-CoV cases by country [total of 19], as of 16May14.
Middle East
Saudi Arabia: 511 cases / 160 deaths
United Arab Emirates: 67 cases / 9 deaths
Qatar: 7 cases / 4 deaths
Jordan: 9 cases / 4 deaths
Oman: 2 cases / 2 deaths
Kuwait: 3 cases / 1 death
Egypt: 1 case/ 0 deaths
Yemen: 1 case/ 1 death
Lebanon: 1 case / 0 deaths
Europe
UK: 4 cases / 3 deaths
Germany: 2 cases / 1 death
France: 2 cases / 1 death
Italy: 1 case / 0 deaths
Greece: 1 case/ 0 deaths
Netherlands: 2 cases / 0 deaths
Africa
Tunisia: 3 cases / 1 death
Asia
Malaysia: 1 case / 1 death
Philippines: 1 case / 0 deaths
Americas
United States: 2 cases / 0 deaths
Since the update of 30Apr14, the geographical range of reported cases has continued to expand, with Lebanon, the Netherlands, and the U.S. reporting their first-ever confirmed cases. In total, roughly 200 confirmed cases have been documented sin the 30Apr14 report and the intervening days since 16May have seen many additional cases noted. These numbers suggest that the explosive rate of new cases observed in April remains in place (see the figure, below, for a time line of reported cases globally).
Distribution of confirmed cases of MERS-CoV by month of onset and place of probable infection, March 2012 - 16 May 2014 (n=621*)
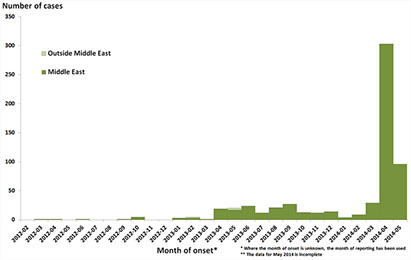
Photo Credit: European CDC
Considerable interest has been sparked by the emergence of a thrid U.S. MERS-CoV case over the past weekend. What is notable about this case is that the patient had only more casual contact (two business meetings and one handshake) with the 1st U.S. confirmed case. Moreover, the third U.S. patient's infection was noted only through serology (detection of anti-MERS-CoV antibodies; case will NOT be officially recognized as a MERS-CoV infection) and the patient is largely asymptomatic. All of these observations raise potential alarm bells concerning the ease of spread and detection of the virus.
An updated summary of the geographical spread of the virus is found in the following figure.
Distribution of confirmed MERS-CoV cases by place of reporting, March 2012 - 16 May 2014 (n=621)

Photo Credit: European CDC
It is interesting that Recombinomics continues to note the existence of a novel subclade of MERS-CoV associated with the April outbreak in Jeddah, a subclade characterized by a set of 11 polymorphisms. Recent sequence data has identified the presence of this subclade in the 2nd U.S. case [but NOT the 1st U.S. case] and in a case from Greece, illustrating the rapid potential spread of a viral species. As also noted by Recombinomics, a very interesting MERS phylogenetic tree has been posted by Andrew Rambaut and the reader is referred to this link. As further noted by Recombinomics, "The above phylogenetic tree supports clonal expansion and sustained transmission which is not limited to hospital settings and instead represents sustained transmission."
Finally, as noted by the ECDC, "The source of MERS-CoV infection and the mode of transmission have not been identified, but the continued detection of cases in the Middle East indicates that there is a persistent source of infection in the region. Dromedary camels are likely an important host species for the virus, and many of the primary cases in clusters have reported direct or indirect camel exposures."
 West African Ebola Outbreak: Update
West African Ebola Outbreak: Update
01May14 Updated 02May14
The WHO has issued an update on the Western Africa Ebola virus outbreak on 28Apr14 and a Communicable Disease Threat update of 02May14. Citing the Ministry of Health (MOH) of Guinea, the update lists a cumulative total of 225 clinical cases of Ebola Virus Disease (EVD) as of 02May14, including 141 deaths. Of these, 41 cases (34 deaths) are listed as probable and 62 cases (35 deaths) are classified as suspected cases. The number of infected health care workers have been revised to 25 (19 confirmed), with 16 deaths (12 confirmed).
Ebola Virions; Image Source: CDC
In an update published a few days earlier, neighboring Liberia is reporting, as of 24Apr14, a total of 35 clinically compatible cases of EVD (6 confirmed cases, 2 probable cases and 27 suspected cases). The last confirmed case was reported on 06Apr14. Meanwhile, the "...Ministry of Health and Sanitation of Sierra Leone is currently investigating 3 patients with an illness compatible with a viral haemorrhagic fever (VHF) for EVD and Lassa fever (the latter is endemic in Sierra Leone)." There have been no confirmed cases of EVD in Sierra Leone.
 U.S. Reports First Case of Imported MERS-CoV
U.S. Reports First Case of Imported MERS-CoV
02May14
The CDC today announced the first confirmed case of human MERS-CoV in the U.S. The patient, from Indiana, is a health care provider who recently traveled to Saudi Arabia. "On April 24, the patient traveled by plane from Riyadh, Saudi Arabia to London, England then from London to Chicago, Illinois. The patient then took a bus from Chicago to Indiana. On the 27th, the patient began to experience respiratory symptoms, including shortness of breath, coughing, and fever. The patient went to an emergency department in an Indiana hospital on April 28th and was admitted on that same day. The patient is being well cared for and is isolated; the patient is currently in stable condition."
The U.S. becomes the 12th country to report a case of MERS-CoV infection.
 Chikungunya Outbreak Expands In Caribbean
Chikungunya Outbreak Expands In Caribbean
01May14 Updated 02May14
The latest update from the ECDC's Communicable Disease Threats Report (as of 26Apr14- Week 17; Also Week 18 update ) shows that the outbreak of Chikungunya in the Caribbean is still expanding, now with over 30,000 confirmed and suspected case. The table below summarizes the current outbreak in various countries in the Caribbean and South America as of 02May14.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 9
Saint Martin 3,160 793 3
Sint Maarten - 301
Saint Barthelemy 485 135
Guadeloupe 8,000 1,328 1
Martinique 19,700 1,515 2
French Guiana - 65
Dominica 1,252 105
Anguilla - 33
Aruba - 1
St. Lucia 1
St. Kitts & Nevis - 1
Saint Vincent
& Grenadines 24 3
Dominican Republic 3,015 17
The geographical range of the virus now spans a considerable part of the Caribbean and a foothold in northeastern South America (see map, below).

Photo Credit: European CDC
The continued expansion of the Chikungunya outbreak in the Americas is fueling increasing worries. At the end of April, officials in the Dominican Republic announced that the actual figure for Chikungunya infections in the country was closer to 3,500 suspected cases. Yesterday, the Public Health minister of the Dominican Republic warned that the country "...faces a chikungunya epidemic". Other Caribbean Health Ministers have stated that they "cannot stop" the spread of the disease even while Haiti has announced it is awaiting confirmation of its first cases.
In the US, the CDC continues it preparations for the eventual spread of the virus here. For an interesting perspective on preventative actions for the US, take a look at this blog post.
 West African Ebola Outbreak: Update
West African Ebola Outbreak: Update
01May14 Updated 02May14
The WHO has issued an update on the Western Africa Ebola virus outbreak on 28Apr14 and a Communicable Disease Threat update of 02May14. Citing the Ministry of Health (MOH) of Guinea, the update lists a cumulative total of 225 clinical cases of Ebola Virus Disease (EVD) as of 02May14, including 141 deaths. Of these, 41 cases (34 deaths) are listed as probable and 62 cases (35 deaths) are classified as suspected cases. The number of infected health care workers have been revised to 25 (19 confirmed), with 16 deaths (12 confirmed).
Ebola Virions; Image Source: CDC
In an update published a few days earlier, neighboring Liberia is reporting, as of 24Apr14, a total of 35 clinically compatible cases of EVD (6 confirmed cases, 2 probable cases and 27 suspected cases). The last confirmed case was reported on 06Apr14. Meanwhile, the "...Ministry of Health and Sanitation of Sierra Leone is currently investigating 3 patients with an illness compatible with a viral haemorrhagic fever (VHF) for EVD and Lassa fever (the latter is endemic in Sierra Leone)." There have been no confirmed cases of EVD in Sierra Leone.
 Saving the Bacon – Global Spread of a Corona Virus
Saving the Bacon – Global Spread of a Corona Virus
17Apr14
Considerable attention has been focused, especially recently, on the SARS-like MERS-CoV outbreak currently afflicting the Middle East. Much of this concern is about the possible global spread of the disease. However, events surrounding the global spread of another corona virus, Porcine Epidemic Diarrhea Virus [PEDV], provide a valuable case study that may be useful in pondering MERS-CoV.
PEDV was first identified in Britain in 1971, subsequently causing widespread epidemics in Europe before arriving in Asia, where it became endemic in the early 1980’s. The disease causes high mortality in piglets (approaching 100%; newborn piglets do not have any protective immunity) but only limited mortality in older animals (less than 3%, though the animals are symptomatic). The virus does not infect humans.

Image Source: Scott Bauer, U.S. Department of Agriculture
PEDV first entered the US last year despite vigorous prevention efforts and over the past year has killed as many as 6 million pigs, mainly piglets. In March, Arizona became the 27th state affected by PEDV. The disease has now extended its reach into Mexico and Canada.
According to a Univ. of Minnesota Fact Sheet, the virus “…can be transmitted by the direct or indirect fecal-oral route. While the direct route would involve animal to animal contact, the indirect route may include contaminated fomites such as footwear, clothing, farm supplies, and vehicles.” The transmission chain of infection is still unknown, but recently attention has focused on the role of porcine plasma, placed in pig feed for its protective role against other infections, as a possible transmission vehicle as well as feral hogs.
A report last fall on the origin, evolution, and genotyping of PEDV in the U.S. observed that “Genetic and phylogenetic analyses of the three U.S. strains revealed a close relationship with Chinese PEDV strains and their likely Chinese origin.” However, the U.S. does not import pigs from China, nor for that matter does Canada which is the largest pig imported for the U.S., so the epidemiological pathway from China to the U.S. is likely more complex than simple importation of diseased animals or animal products. One intriguing clue as to the geographic spread of PEDV to the U.S. was noted in the cited scientific study: “…that the emergent U.S. PEDV strains share unique genetic features at the 5'-untranslated region with a bat coronavirus provided further support of the evolutionary origin of PEDV from bats and potential cross-species transmission.” Like MERS-CoV, the hunt to define infection source and transmission chain pathways is difficult and currently enigmatic.
While humans are not infected by PEDV, they do feel the impact of its existence: an economic impact of the virus is already felt. Current forecasts are for U.S. hog production to shrink anywhere from 3-7%, although recent data seems to indicate a lesser impact of the virus this winter. The PEDV outbreak in the U.S. has already resulted in the biggest drop in pork production in 30 years and much higher pork-related food costs for consumers as well as considerable economic hardship for producers. The consequences of the PEDV outbreak are potentially severe enough that the USDA has announced that it will now require disease reporting in an effort to enhance surveillance.
 MERS-CoV Cases Now in Malaysia and the Philippines
MERS-CoV Cases Now in Malaysia and the Philippines
16Apr14
Fresh on the heels of this past weekend's news of the first reported human case of MERS-CoV infection in Yemen, the first reports of human infection in two new countries have been announced today. A nurse, recently returned (4/15) from the United Arab Emirates to the Philippines has tested positive for the MERS-CoV virus according to news reports. When last in the UAE, the nurse was reportedly been "exposed to the Filipino paramedic who died from the disease in Al Ain". The subject, plus 9 other close contacts, have not exhibited symptoms of MERS-CoV infection but have been placed under quarantine. The Philippine government has issued a MERS-CoV advisory.
At the same time, news reports out of Malaysia cite the first known case of human infection by MERS-CoV in a man from Batu Pahat, Johor. The patient has reportedly died from the infection, having recently "returned to Malaysia from performing umrah and arrival on 29 March 2014. On 8-9 April 2014, he experiences symptoms fever, cough and difficulty breathing. On 10 April 2014, he was admitted to Sultanah Nora Ismail (HSNI), for the inspection and further treatment. Circumstances he became increasingly ill and confirmed died the world on 13 April ...." the determined cause of death was "...Severe Pneumonia Secondary to MERS-CoV".
Cases of MERS-CoV appear to be continuing their upward spike. A posting today at the blog Avian Flu Diary, citing press releases from the Saudi Ministry of Health, notes an additional 11 confirmed cases of MERS-CoV infection, including two fatalities, in the last 48 hours. Also, today, the WHO reported on a UAE "...cluster of ten laboratory-confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection among health-care workers identified through screening of contacts of a previously laboratory-confirmed case from Abu Dhabi who died on 10 April 2014." A rapidly expanding case count coupled with an increasing geographic spread is a worrisome combination that could herald a significant expansion of the MERS-CoV outbreak.
 W. African Ebola Virus Out-break: April 14th Update
W. African Ebola Virus Out-break: April 14th Update
14Apr14
The latest data from the WHO's African Regional Office, in a Epidemic and Pandemic Alert and Response (EPR) dated 14Apr14,
updates the tally of Ebola virus disease (EVD) in west Africa to a cumulative total of 200 clinically compatible cases including 119 deaths.
Guinea continues to be the hardest hit country with a total of 168 clinically compatible cases of Ebola virus disease (EVD), including 106 deaths. A total of 6 districts in Guinea have reported cases including Conakry, with 31 clinically compatible cases, 22 of which are laboratory confirmed. "A total of 71 clinical cases have been laboratory confirmed (45%), while 34 of the remaining clinical cases are classified as probable cases and 54 as suspected cases. Forty-two of the 106 deaths (40%) have been laboratory confirmed." Sixteen of the 168 clinically compatible cases have occurred in health care workers.
The tally of EVD in Liberia has increased to a cumulative total of 6 laboratory confirmed cases and 20 suspected cases. A total of 13 deaths in patients with clinically compatible EVD have been reported in Liberia, 6 of these are laboratory confirmed cases. The situation in Mali remains unchanged since the prior report on 11Apr14: a total of 6 suspected cases of EVD, though no confirmed cases. Countries such as Sierra Leone and the Ivory Coast remain on high alert.
The salient features of this outbreak that are causing concern are: 1) the viral stain is the highly virulent Zaire strain of Ebola; 2) the rapid geographic spread of the outbreak, and 3) the foothold of EVD in a major city, Conakry, the capital and largest city of Guinea with a population over 1.5 million. Ebola transmission requires direct contact through contaminated bodily fluids from infected humans or animals (bats are a natural reservoir for the virus), so Ebola outbreaks in rural areas have huge impediments to growth. However, EVD in a major city with its intrinsically higher population density is potentially another matter.

Image Credit: CDC
As noted in a WHO background document, "The incubation period, the time interval from infection with the virus to onset of symptoms, is 2 to 21 days. People remain infectious as long as their blood and secretions contain the virus, a period that has been reported to be as long as 61 days after onset of illness." The current outbreak in Western Africa could be with us for some months to come.
 U.S. Flu Activity, Week 14: A Flu B Bounce for Spring
U.S. Flu Activity, Week 14: A Flu B Bounce for Spring
13Apr14
The latest data from the CDC for the week ending April 5th (week 14) has been published. The data shows that flu activity in the U.S. has taken a recent upturn due to a notable surge in influenza B activity even as influenza A/H1N1p all but disappears (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased slightly for the third week in a row to 13.4% nationally, compared to 12.5% the prior week and 11.5% the week before. Regions 1-6 had percent flu positive values in excess of the national rate, while Regions 7-10 were well below the national rate. In particular, Regions 1-3, with percent positive samples at 26.4%, 23.4%, and 18.4% respectively, comprise the hardest hit areas. The following graph illustrates the overall trends by region for % flu positive samples this season.
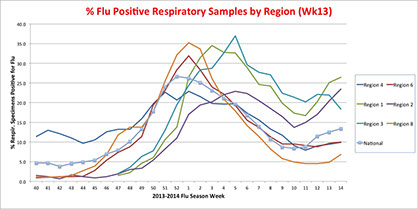
The pneumonia and influenza (P&I) mortality index for Week 14 is 6.8% (6.5% for Week 13), below the epidemic threshold of 7.3%. There were three influenza-associated pediatric deaths reported, one ascribed to not-subtyped influenza A while the other two fatalities were ascribed to influenza B. Three influenza-associated pediatric deaths were reported the preceding week. A total of 85 influenza-associated pediatric deaths have been reported this season.
The proportion of outpatient visits ascribed to influenza (ILI) was 1.6% (versus 1.6% the prior week), again below the national baseline of 2%. The distribution of ILI activity-by-state again shows only NYC with “high ILI activity” (see table below) and one state with "moderate ILI activity". When typed, only 44.1% of isolates were influenza A while 55.9% were influenza B. Roughly 60% of influenza A specimens were subtyped, the majority of these (2/3) were identified as A/H3N2 and 1/3 as 2009 H1N1p.
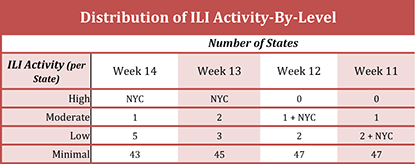
While only 1 of the 1,657 antigenically characterized 2009 H1N1p isolates examined this year season has shown reduced titers with antiserum produced against A/California/7/2009 [the current vaccine strain for 2009 H1N1p], nearly 2% of H3N2 viruses (5/264) showed reduced titers with antiserum produced against A/Texas/50/2012, the influenza A (H3N2) component of the 2013-2014 Northern Hemisphere influenza vaccine.
The number of Tamiflu-resistant isolates detected this season increased to 52 (up 1 from the preceding week) and the % of tested isolates found to be Tamiflu-resistant remained at 1.2%. By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
Earlier this season and in contrast to normal "seasonal" flu, the predominance of the 2009 H1N1p virus this season led to a shift in the demographic of patients most affected: at one point people 18-64 years accounted for more than 60% of reported hospitalized cases. As the incidence of 2009 H1N1p has declined to very low levels over the past weeks, nonetheless people 18-64 years still account for approximately 60% of reported influenza-associated hospitalized cases for the season. This demographic clearly distinguishes this season from a "typical" one dominated by seasonal flu.
The recent increase in the proportion of flu cases ascribed to influenza B is not unexpected and will likely continue well into the spring. However, its magnitude is somewhat surprising, as is its apparent geographical concentration in the Northeast. Indeed, inspection of the graph, above, illustrating percent flu-positive respiratory samples by region and time shows that the current season has been comprised of distinct geo-temporal "waves". Regions 1-3 appear to have had a later seasonal peak and a much higher influenza B "Spring bounce" as compared to, for example, Regions 6 or 8. It is interesting to note that recent data out of Canada also shows late season influenza B activity concentrated in Ontario and Quebec, supporting the Eastern geographical concentration observed in the U.S.
 Ebola Virus Outbreak in Guinea Kills At Least 59
Ebola Virus Outbreak in Guinea Kills At Least 59
24Mar14
A news report from the BBC cites 59 deaths in an outbreak of Ebola virus in the remote forest region of south Guinea while noting that two suspected cases in the capital city of Conakry, where the victims died from an unknown hemorrhagic fever, tested negative for the deadly virus. A similar report from the Australian Broadcasting Corporation also relates that the outbreak began in Guinea around Feb. 9th and now has affected some 80 patients. As noted in the BBC article, the current Ebola outbreak is the first for Guinea, while pointing out that “Recent cases have been thousands of miles away, in Uganda and Democratic Republic of Congo.”
A posting Saturday on ProMed Mail noted that sequencing of the Ebolavirus L gene from clinical isolates from Guinea showed strong homology to Zaire Ebolavirus, “considered the most lethal species” of the virus with case fatality rates of up to 90%. Other species of Ebolavirus include Bundibugyo, Ivory Coast, Reston, and Sudan. “Bundibugyo, Sudan and Zaire species have been associated with large Ebola haemorrhagic fever (EHF) outbreaks in Africa..”, according to ProMED Mail. The presence of the Zaire species of Ebolavirus in Guinea casts a shadow of suspicion that the Zaire species is responsible for the Ebola cases reported in nearby Sierra Leone.
As noted in the ABC report, “Ebola, one of the world's most virulent diseases, was first discovered in the Democratic Republic of Congo (DRC) in 1976 and the country has since had eight outbreaks.The most recent epidemic in the DRC infected 62 people and left 34 dead between May and November 2012, according to the country's health ministry.”
 Chikungunya Outbreak In Caribbean Continues
Chikungunya Outbreak In Caribbean Continues
24Mar14
The outbreak of chikungunya virus in the Caribbean continues, though the rate of new cases may be diminishing. According to the latest Communicable Disease Threats Report (of 21Mar14) from the European CDC, there have been more than 15,000 probable and confirmed cases in the region including five fatalities. The table below summarizes the current outbreak in various countries in the Caribbean.
Suspected Cases Confirmed Cases Deaths
Virgin Is. (UK) 7
Saint Martin- 2,640 782 3
Sint Maarten - 115
Saint Barthelemy - 420 134
Guadeloupe - 1,960 586
Martinique - 7,630 1,141 2
French Guiana - 32
Dominica 394 56
Anguilla - 14
Aruba - 1
St. Kitts & Nevis - 1
Chikungunya is transmitted by the mosquito Aedes aegypti, as are related arboviruses such as dengue, West Nile, and Eastern Equine Encephalitis virus. In 2006, a mutated version of the chikungunya virus was found in an outbreak in Reunion Island that allowed more ready transmission in another mosquito strain, the aggressively invasive Aedes albopictus. [As an aside, Ae. albopictus is already found in the SE United States and continues to expand northward (see this reference)]. This mutation enhanced the geographical spread of the virus, as did the continued global spread of both mosquito strains, most recently into the Caribbean (see map of global Ae. albopictus, below, where blue areas show original distribution and green areas show those populated since 1977). The first cases of chikungunya in the Caribbean were reported early last December from the island St. Martin. Health officials have expressed concern about the potential spread of chikungunya virus to the North American continent.

Photo Credit: By Gancho (Own work) [GFDL], via Wikimedia Commons
 MERS-CoV Case Count Now Over 200
MERS-CoV Case Count Now Over 200
24Mar14
The European CDC is reporting that the number of laboratory-confirmed human cases of the SARS-like MERS-CoV infection now stands at 201 with 85 fatalities. The Kingdom of Saudi Arabia continues to be the hardest hit with 159 laboratory-confirmed cases and 64 fatalities. The following table from the ECDC report breaks down the distribution of MERS-CoV cases by country.
Saudi Arabia: 159 cases / 64 deaths
United Arab Emirates: 15 cases / 5 deaths
Qatar: 7 cases / 4 deaths
Jordan: 3 cases / 3 deaths
Oman: 2 cases / 2 deaths
Kuwait: 3 cases / 1 death
UK: 4 cases / 3 deaths
Germany: 2 cases / 1 death
France: 2 cases / 1 death
Italy: 1 case / 0 death
Tunisia: 3 cases / 1 death
The rate of new cases appears to have abated somewhat from its peak levels last Fall, but may be increasing as we head into Q2 for 2014, as shown in the summary slide below from the ECDC report.
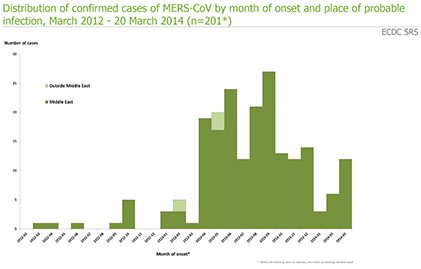
Photo Credit: European CDC
While there have been instances of local transmission among patients, for example in France and the UK, the risk of secondary transmission in these countries remains low. More generally, person-to-person transmission has been noted among close contacts and health care providers. However as noted in the ECDC report, the extent of secondary transmission has been limited. Of course the single largest issue looming over this outbreak is that the source and mode of transmission have yet to be identified, though recent work is currently pointing towards a potential role for camels in the etiology of the disease.
 Learning from the Boston HIV Mystery
Learning from the Boston HIV Mystery
11Mar14
Results presented in the waning days of the annual Conference on Retroviruses and Opportunistic Infections [CROI] by Dr. Tim Henrich (Brigham and Women's Hospital, Boston) has prompted a fascinating article by Michael Smith, MedPage Today's North American correspondent. The subject of the article are two HIV patients known as "the Boston patients.
These two HIV patients were first noted in 2012 and again last year at the 7th International AIDS Society meeting on HIV pathogenesis, treatment, and prevention in Kuala Lumpur. In brief, the male HIV patients received allogeneic bone marrow transplants that resulted in "...almost complete eradication of HIV throughout their body..." In 2012, the two patients were still on anti-retroviral therapy, but last year were reportedly off antiretroviral drugs for several weeks without evidence of viral rebound. Both patients had undergone bone marrow transplantation for the treatment of cancer and in neither case did the donor cells contain the CCR5 delta32 mutation (that renders T cells resistant to HIV infection) though both patients are themselves heterozygotes for the mutation. Both patients were able to remain aviremic for extended periods of time (4 years or 2 years, respectively) as long as anti-retrovirals were taken.
This years update focused on the consequences of treatment interruption in these patients. As stated in Michael Smith's article: "The bottom line appears to be this: an allogeneic stem cell transplant can make HIV almost undetectable and lead to remission -- without antiretroviral therapy -- "of variable duration."" The noted durations before onset of an acute HIV infection were 12 weeks for one patient and 8 months for the other.
The results are intriguing but far from clear. As noted in the article, there are many variables at play in this approach and systematic evaluation will be necessary to glean exactly what is going on. But the observations are compelling, in a manner reminiscent of immunology experiments in the mid-20th century that were often driven by phenomenology as investigators wrestled to understand underlying principles.
 Tackling HIV With Gene Editing
Tackling HIV With Gene Editing
06Mar14
The latest issue of the New England Journal of Medicine contains a remarkable article that brings synthetic biology and “personalized medicine” to the forefront of anti-HIV therapeutics under study. In brief, the authors of this study, led by Dr. Carl June at UPenn, performed “gene editing” on immune cells from HIV-infected individuals to eliminate the major co-receptor of HIV, CCR5, required for infection of T-cells. In an open-label, nonrandomized, uncontrolled study, patients with chronic aviremic HIV infection received a single dose of modified, autologous immune cells. These patients were subsequently found to have increased T-cell counts and, in one patient, HIV RNA levels became undetectable.
This research work was driven by prior clinical observation of HIV in patients with the CCR5-delta32 deletion, a natural mutation with 32 base pairs of the CCR5 gene deleted. Individuals homozygous in CCR5-delta32 are refractory to HIV infection (reference) while heterozygotes show a slower disease progression (reference). In certain populations, 10-20% of individuals may be heterozygous for CCR5-delta32. These observations prompted, in part, the development of new small molecule HIV entry inhibitors, such as maraviroc (reference). Further, one HIV-infected transplant recipient who received cells from a CCR5-delta32 homozygous donor was reported as effectively “cured” of HIV infection (reference). Thus, CCR5 is an excellent target for “gene editing” therapy.
To accomplish this, the authors employed one of several available technologies to edit the target genome – zinc finger nucleases (ZFNs) specifically engineered to target the CCR5 gene. ZFNs have two parts: a buzz saw-like nuclease and DNA recognition domains. The utility of ZFNs resides in what happens after nuclease cleavage of the target gene: repair. As explained in the article, “….the DNA can be repaired by either homologous recombination or nonhomologous end joining. Homologous recombination repairs the break while preserving the original DNA sequence. However, these cells are susceptible to recutting by ZFNs. In contrast, nonhomologous end joining can result in random insertion or deletion of nucleotides at the break site, resulting in permanent disruption of the primary DNA sequence.” In other words, a functional knockout or knockdown is created.
ZFNs are packaged into an adenoviral delivery system and used to transduce immune cells derived from the patient ex vivo.
The actual trial construct and concurrent clinical observations in this study are even more interesting than the headline. The study was composed of 12 aviremic HIV patients who had been receiving highly active anti-retroviral therapy (HAART). Patient response to HAART segregated into two cohorts: six with restored CD4+ T-cell counts above 450 cells/mm3 [immune responders] and six whose restored CD4+ T cell counts remained between 250-500 cells/mm3 [immune non-responders] with a minimum duration of HAART for 2 years. All twelve patients received reinfusion of autologous, genetically edited immune cells (5-10 billion cells). All patients were followed for 252 days post-reinfusion. Patients in the cohort of immune responders were, after one-month post-reinfusion, subject to a 12 week interruption of HAART. A control group of eight aviremic HIV patients was also employed. The primary objective of the study was “to assess the safety and tolerability of a single dose of autologous CD4 enriched T cells” with a modified CCR5 gene.
This was indeed the case. T cell counts in treat patients increased, transiently, nearly three-fold. And while HIV viremia resurfaced in the first cohort after temporary cessation of HAART, the decline in CCR5 modified cells was less than that of unmodified cells (again, about 3-fold less). Indeed, “HIV RNA became undetectable in one of four patients who could be evaluated.” One week after autologous transplantation, fully 14% of circulating CD4 T cells were CCR5-modified cells. Modified T-cells were also found in the rectal mucosa of all treated patients.
However, the larger question is whether this approach can show efficacy and this will require further clinical study. In an accompanying editorial, Drs. Mark Kay and Bruce Walker note that “For this approach to become clinically useful as treatment for HIV infection, biallelic CCR5 knockout will be required. It was interesting to note that the study participant in whom the viral load fell to undetectable levels was later found to be heterozygous for the CCR5-delta32 deletion — and therefore did not require biallelic knockout.”
The problem is that biallelic knockouts in the realm of autologous immune cell transplantation are not yet feasible. Technically, biallelic knockouts have been achieved (see here or here or here for examples from the xenotransplantation field) but these involve the combined use of a gene editing nuclease (TALENs or ZFNs or CRISPR] with other techniques such as somatic nuclear transfer.
Nonetheless, this study opens the door to a new line of defense against HIV. The present study is just one of several related approaches that could utilize the same technology. As noted by the study authors, “Our strategy is to repopulate the immune system with CCR5-deficient central memory T lymphocytes by infusion of SB-728-T. Alternative approaches that are promising include infusions of autologous CCR5-modified hematopoietic stem cells, stem-cell transplantation procedures, and the use of CCR5-specific ribozymes and short hairpin RNA.” The successful completion of a clinical safety and tolerability study is an important milestone in exploring these new approaches to HIV control without chronic drug regimens.
 U.S. Flu Activity in Week 7: High But Slowly Ebbing
U.S. Flu Activity in Week 7: High But Slowly Ebbing
24Feb14
The latest data from the CDC for the week ending February 15th (week 7) has been published. The data shows that flu activity in the U.S. again is still robust, though most indicators were once again down slightly from the week prior (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza fell again to 13.9% nationally, compared to 16.8% the prior week and 19.6% the week before. All regions had percent flu positive values in excess of the national rate, save Regions 6 [AR, LA, NM, OK, TX], 7 [IA, KS, MO, NE], 8 [CO, MT, ND, SD, UT, WY] and 10 [AK, ID, OR, WA] at 15.5%,15.0%, 14.2% and 16.4% respectively. The following graph illustrates the overall trends by region for % flu positive samples this season. In particular, Regions 1,3,& 5 still are exhibiting percent positive values around 29% and thus comprise the vaward of current influenza activity in the U.S.
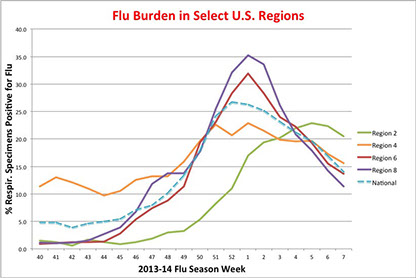
The pneumonia and influenza (P&I) mortality index is 8.2% (8.4% last week), above the epidemic threshold of 7.4% for Week 7. There were two influenza-associated pediatric deaths reported, one ascribed to the 2009 H1N1p virus and the other ascribed to not-subtyped influenza A. Ten influenza-associated pediatric deaths were reported last week. A total of 52 influenza-associated pediatric deaths have been reported this season.
The proportion of outpatient visits ascribed to influenza (ILI) was 2.5% (versus 3.0% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows no states with “high ILI activity” (see table below) and seven states with "moderate ILI activity". When typed, the majority of isolates were influenza A (~90% of typed specimens) and, while only 52% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 97%; 3% were H3N2).
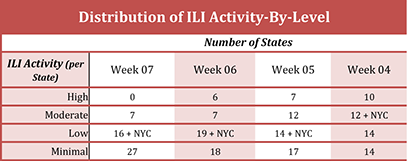
The number of Tamiflu-resistant isolates detected this season increased to 26, and the % of tested isolates found to be Tamiflu-resistant fell slightly to 0.7% (from 0.8%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
With leading indicators down for a sixth week in a row, there is a high likelihood that the influenza season has already peaked for the season, though the nation still remains firmly in the grip of an active season. In contrast to a normal "seasonal" flu, the predominance of the 2009 H1N1p virus this season has led to a shift in the demographic of patients most affected: people 18-64 years accounted for more than 60% of reported hospitalized cases.
Thus, the ebbing tide of influenza will continue as a "high impact" virus this season. For example, researchers from the CDC and the California Department of Public Health reported in last week's MMWR on the high impact of this year's flu season on California which, through mid-January, has resulted in 405 severe cases, two thirds of which were in patients 41-64 years of age. During this same period, 94 deaths and 311 ICU submissions were tallied. However, by last Friday, California officials were reporting 243 confirmed deaths with 41 additional "likely" fatalities under investigation. This is the highest influenza-related death toll since the 2009 pandemic outbreak. In a telling statistic, only 6 of the 28 fatalities where vaccination records were available had been immunized. Thus, the CDC is still urging people to get vaccinated even now; there are many weeks left to the current flu season.
The recent, slow increase in the proportion of flu cases ascribed to influenza B is not unexpected and will likely continue well into the spring.
 U.S. Flu Activity in Week 2: Peaked (Hopefully) Already?
U.S. Flu Activity in Week 2: Peaked (Hopefully) Already?
19Jan14
The latest data from the CDC for the week ending January 11th (week 2) has been published. The data shows that flu activity in the U.S. again is still robust, though some indicators were again down slightly from the week prior (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza fell again to 25.1% nationally, compared to 26.2% the prior week and 26.7% the week before. All regions had percent flu positive values in excess of the national rate, save Regions 2 [NJ, NY, Puerto Rico, US Virgin Islands] and 4 [AL, FL, GA, KY, MS, NC, SC, TN], at 19.4% and 21.5% respectively.

The pneumonia and influenza (P&I) mortality index is 7.5% (6.9% last week), above the epidemic threshold (for the first time this season) of 7.2% for Week 2. There were ten influenza-associated pediatric deaths reported: seven that were ascribed to 2009 H1N1p, two ascribed to not-subtyped influenza A, and one was associated with non-typed influenza. The marked up-tick in both of these lagging indicators underscores the apparent clinical severity of many flu cases this season.
The proportion of outpatient visits ascribed to influenza (ILI) was 3.6% (versus 4.4% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows fourteen states with “high ILI activity” (see table below) and twelve with "moderate ILI activity". When typed, the majority of isolates were influenza A (~98% of typed specimens) and, while only 67% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 97%; 3% were H3N2).
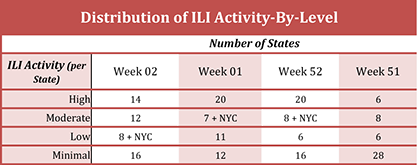
The number of Tamiflu-resistant isolates detected this season remained at 13, and the % of tested isolates found to be Tamiflu-resistant fell to 0.8% (from 1.3%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
With leading indicators down for a second week in a row, it remains to be seen whether influenza will resume its earlier upward trend in the coming weeks. Many of the most populated regions of the country have yet to feel the full brunt of the flu and there is no reason to think they won't. In particular, the east coast has only seen higher levels on influenza in the Carolinas and Virginia (in terms of ILI). If other states along the eastern seaboard, as well as CA, experience higher levels of flu activity, then the number of cases could continue to climb significantly. On the other hand, we could be seeing a marked downturn in H1N1p activity, so look to next week's data for further signs of decline. A rise in H3N2 may be possible yet plus a late-season persistence in flu B cases (as is typical) will undoubtedly keep flu season active till the Spring. But a third consecutive down tick next week in the leading indicators would offer considerable hope that the worst this season has passed.
 Confirmed Cases of H7N9 Jump to 205, at Pace With Last Spring's Peak Rate
Confirmed Cases of H7N9 Jump to 205, at Pace With Last Spring's Peak Rate
19Jan14
The global number of confirmed cases of human infection by influenza H7N9 has swollen to 205 with 54 fatalities. Nine new cases were reported in Zhejiang Province, three each in Fujian and Guangdong Provinces, and an additional case was reported in Shanghai. The latest stats and a breakdown of new cases by country & province can be found here. A table with details of confirmed H7N9 cases can be found here.
Perhaps because of the sudden upward spike in confirmed H7N9 cases in China since the start of 2014, ProMED Mail is has published a notice from Hong Kong's Information Services Department stating that "Starting from 24 Jan 2014, Hong Kong and the Mainland will conduct serological testing for H7 avian influenza (AI) on live poultry at Mainland registered farms and the Man Kam To Animal Inspection Station. Serological testing will also be introduced to local poultry farms in Hong Kong on the same day."
While the city of Shanghai has previously announced that live poultry trading will be suspended from 31Jan14 till 30Apr14 to control the H7N9 virus, this newest step represents a considerable escalation of control efforts in Hong Kong and the mainland. the rationale behind these moves is simple, as re-iterated in the ProMED Mail posting: ""The traditional Chinese New Year holiday period is approaching with its associated large-scale population movement and enhanced slaughter and consumption of poultry, which the local and national authorities will have difficulty controlling. During this period there will be enhanced opportunity for the evolution of H7N9 virus with potential for transition from person-to-person."" such market intervention seemed to pay dividends last spring and hopefully shall again.
 Canadian H5N1 Case Draws Close Attention
Canadian H5N1 Case Draws Close Attention
16Jan14
The mystery surrounding the death of an Albertan nurse last week from H5N1 largely remains, but the wheels of investigation are turning. The mystery, in a nutshell, is that a healthy young woman from Canada traveled to Beijing on a family holiday, a locale without any recent human cases of H5N1 influenza, had no apparent exposure to poultry, but nonetheless fell ill from the virus on her return flight and succumbed shortly thereafter. Moreover, her presentation of symptoms was atypical for flu (no extensive respiratory problems - rather the patient presented with encephalitis).
Yesterday, a news report relayed that "Canada's National Microbiology Laboratory has isolated live H5N1 virus from respiratory specimens taken from an Alberta woman..." with the goal "...to sequence the entire genome of the virus..." This is a crucial step in trying to pick apart the mystery around this case.
Also yesterday, the CDC issued a HAN Advisory as a result of the Canadian H5N1 case. The advisory alerts clinicians to the fact that the "...clinical presentation of human infection with avian influenza A viruses varies considerably." Therefore, "Clinicians should consider the possibility of avian influenza A (H5N1) virus infection in persons exhibiting symptoms of severe respiratory illness who have appropriate travel or exposure history."
 Confirmed H7N9 Cases This Season More Than Double in a Week
Confirmed H7N9 Cases This Season More Than Double in a Week
11Jan14
The number of confirmed cases of human H7N9 infection this season (since roughly mid-October last) has doubled in a single week with 19 news cases reported since 04Jan14. Overall, 33 cases have been reported this season including 4 fatalities. The latest stats and a breakdown of new cases by country & province can be found here. A table with details of confirmed H7N9 cases can be found here.
These new cases were announced against a backdrop of additional positive environmental samplings in and around Guangdong Province in China. CIDRAP News is reporting that H7N9 positive samples were found in a restaurant as well as near wet markets in Guangzhou. Interestingly, the restaurant had taken delivery of live chickens by a recently-confirmed H7N9 patient. Also, please see this news story.
Chinese authorities have long warned of a possible up-tick in human H7N9 cases as the New Year begins and have already ordered the closure of all 117 live poultry markets in Shanghai from the end of January through 30Apr14 in an effort to stymie the recurrence of H7N9. However, the expanding number of recent cases may suggest that the planned timing around these market closures may be too late.
 U.S. Flu Activity Spikes Upward in Week 52
U.S. Flu Activity Spikes Upward in Week 52
04Jan14
The latest data from the CDC for the week ending December 28th (week 52) has been published. The data shows that flu activity in the U.S. again increased significantly over the preceding week (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 26.7% nationally, up from 24.1% the prior week. Regions 5 [IL, IN, MI, MN, OH, WI], 6 [AR, LA, NM, OK, TX], 8 [CO, MT, ND, SD, UT, WY], and 10 [AK, ID, OR, WA] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN] and 7 [IA, KS, MO, NE] followed, below the national average at 20.7% and 24.7%, respectively, while the remaining regions were further below the national average.
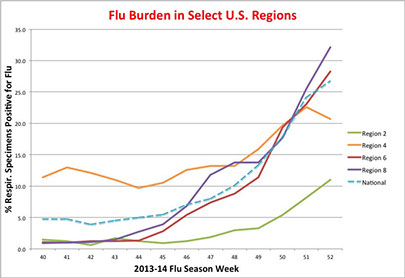
The pneumonia and influenza (P&I) mortality index is 6.5% (6.7% last week), below the epidemic threshold of 7.0% for week 52, and there were two influenza-associated pediatric death reported, ascribed to 2009 H1N1p and to a non-subtyped influenza A, that occurred weeks 51 and 50, respectively. The proportion of outpatient visits ascribed to influenza (ILI) was 4.3% (versus 3% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows twenty states with “high ILI activity” (see table below) and 8 + NYC with "moderate ILI activity". When typed, the majority of isolates were influenza A (~97% of typed specimens) and, while only 55% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 99%; 0.4% were H3N2).
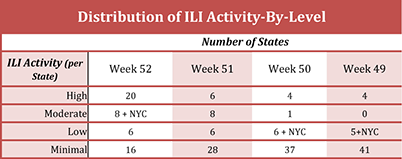
The number of Tamiflu-resistant isolates detected this season remained at 10, and the % of tested isolates found to be Tamiflu-resistant fell to 1.1% (from 1.3%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
The flu season has come on strongly the past few weeks. And it is clear that the target population (young and middle-aged adults; see the CDC advisory of 12/24) and severity of the infection is/can be distinct from the preceding years. However, it is still not clear if this season's flu season will any more severe than last year's, which was a bad session of seasonal (mainly H3N2) flu. For example, a local news report out of SC tells of 14,000 cases of flu so far this season with 800 hospitalizations and 9 deaths. "But this season isn’t as bad as last season. In the last week of 2012, South Carolina had already reported 15 deaths and almost 33,000 flu cases."
This is not to minimize the severity of what we are observing now. It is just too early to forecast how bad this season will be. This site has been sounding notes of caution over the 2009 H1N1p virus for the past year, as it ravaged other parts of the world - especially India, and many important questions need to be answered, most notably any genetic changes in the virus that might underlie increased virulence and/or mortality. On the other hand, we have already seen a reduction this past week in the % of flu-positive respiratory samples in region 4, which has previously been above the national average for most of the season. Is this the result of the just-passed holiday season suppressing the stats or might it be an early sentinel that a peak in flu activity is just around the corner, say in mid-late January? Last year's flu season came early and peaked at Week 52. But the 2007-2008 season, also a bad year, didn't peak until around week 8. It is not yet clear where this season will fall between these two scenarios.
In either event, the best advice remains to get vaccinated.
 A Newly Confirmed Case of Flu A/H7N9 in Shanghai
A Newly Confirmed Case of Flu A/H7N9 in Shanghai
04Jan14
The official Chinese news agency, Xinhua, is reporting online yet another confirmed case of human H7N9 infection, this time in the city of Shanghai. The patient (86M) was confirmed with H7N9 yesterday and is currently hospitalized for treatment. No other details are currently available. this latest case increase the number of confirmed cases this season to 14 with one fatality. Since the onset of human H7N9 infections last spring, 149 confirmed cases have been reported with 46 fatalities.
In the bubbling cauldron of influenza strains currently percolating in South Asia, a new dimension has emerged. Reports (see here and here) have emerged of a new outbreak of avian H5N1 in southwestern China and in India. More fodder for potential influenza recombinants.
 A 2nd Case of Human H9N2 Flu Infection This Season
A 2nd Case of Human H9N2 Flu Infection This Season
02Jan14
A posting on ProMED mail tells of a 2nd confirmed human infection with the H9N2 avian influenza virus. The patient (7M) is from Hunan Province in China, was in contact with poultry, and fell ill on 19Nov13. He has recovered after treatment in hospital.
This new case apparently antedates an earlier report of the first confirmed H9N2 case in Hong Kong in four years, that of an 86M from Shenzhen City in Guangdong Province. That patient was hospitalized on 28Dec13 and is currently in stable condition and is afebrile.
As noted in the ProMED report, “H9N2 is an avian flu subtype that mainly affects ducks and chickens but can also pass to humans, causing mild symptoms. Under Hong Kong law cases of such infection must be made public…” Overall, this is the 7th confirmed case in Hong Kong since 1999.
 A 2nd Confirmed Case of H7N9 Flu in Taiwan
A 2nd Confirmed Case of H7N9 Flu in Taiwan
01Jan14
A ProMED mail posting is reporting that a 2nd person in Taiwan, an 86M traveling in Taiwan from Jiangsu Province, fell ill on 19Dec13, two days after entering Taiwan. He was hospitalized on 24Dec13 with pneumonia and placed on a ventilator. Citing Taiwan’s Central News Agency, the posting notes that “this patient's symptoms were slightly different from previously reported infections, indicating that doctors still face some difficulty in diagnosing the virus, he added. The man's infection could mean that H7N9 has become prevalent across all of southern China even though, puzzlingly, major duck and chicken farms in the region have been found disease-free.”
It appears likely that the patient was infected with H7N9 prior to entering Taiwan. Nonetheless, the only other confirmed case of human H7N9 infection was recorded last spring. Also of interest, the patient was part of a 25-person tour group, most of whom have since returned home.
This case raises the global count of confirmed H7N9 influenza infections in humans to 148 with 46 fatalities.
 Chikungunya Outbreak Grows in Carribean
Chikungunya Outbreak Grows in Carribean
01Jan14
The first-ever outbreak of chikungunya virus infections in humans in the Caribbean continues to grow, as reported just before the New Year by CIDRAP News. Citing a Dec. 28th report by the European Centre for Disease Prevention and Control, the article reports that the island of St. Martin has seen a spike in chikungunya cases, with the number of confirmed cases jumping from 22 to 66. In addition, a first case has now been reported on the Dutch side of the island while the nearby islands of Guadeloupe and Martinique have reported an additional four cases.
More confirmed cases from the Caribbean are likely as authorities investigate numerous reports of suspect and probable cases. The CIDRAP News report cites 167 suspected cases on the French part of St. Martin, 27 on Martinique, and 21 on St. Barthelemy.
The CDC has issued a HAN advisory as well as a notice to travelers on Dec. 13th. Given the identity of the mosquito vectors employed by the virus (Aedes aegypti and A. albopictus), there is a real concern for eventual cases on the U.S. mainland, such as was observed for another, related viruses - dengue fever virus and West Nile virus.
 Hong Kong Reports 1st Seasonal Fatality From Flu A/H7N9
Hong Kong Reports 1st Seasonal Fatality From Flu A/H7N9
25Dec13
Hong Kong is reporting its first fatality from H7N9 flu. The patient (80M) died today. See a press report here. This is the first H7N9 fatality, globally, of the 2013-14 season.
 A Year of Firsts for Influenza: Flu A/H10N8 Claims Its First Known Human Fatality
A Year of Firsts for Influenza: Flu A/H10N8 Claims Its First Known Human Fatality
18Dec13
It has been an impressive year of “Firsts” for influenza. Among this years list of “first-ever” events are the outbreak of A/H7N9 that began last spring and continues even now. There was also the first-ever reported case of human infection by A/H6N1, which occurred earlier this year in Taiwan. Now comes news of the first ever case of a human fatality due to influenza A/H10N8 Infection (see press reports here and here, as well as remarks from the WHO).
The patient (73F) lived in Jiangxi Province and passed away on 06Dec13 from respiratory failure. Her symptoms included severe pneumonia, respiratory distress, high blood pressure, as well as a neuromuscular disorder. The patient had a variety of underlying medical conditions (i.e. patient was immuno-compromised).
The source of the infection is unknown. The patient had been to a live bird market four days prior to the onset of symptoms. Influenza A/H10N8 is considered a low pathogenicity avian influenza virus most prevalent in aquatic waterfowl.
Just last year, a team from the College of Veterinary Medicine, South China Agricultural University and the Guangzhou Animal Health Inspection Institute reported [ http://jvi.asm.org/content/86/14/7716.full ] a complete genomic sequence on a A/H10N8 isolate obtained, for the first time, from a live bird market (duck)in Guangdong Province.
Why is this a concern and not just an oddity detected by chance due to enhanced flu surveillance in China? Part of the answer can be found in a paper published in 2011 which studied an H10N8 isolate from the Dongting Lake wetland reservoir, an important site for East Asian migratory birds. The results in the paper showed that while the virus was only of low pathogenicity for chickens, it replicated efficiently in the mouse lung without prior adaptation, and the virulence to mice increased rapidly during adaptation in mouse lung. Indeed, the virus became lethal after only two passages in the lung. Such observations suggest a low barrier for some LPAIs to become mammalian pathogens of high pathogenicity.
As noted by these investigators, an earlier study had demonstrated direct transmission of an influenza A virus directly from wild birds to humans, in this case “…influenza A/H11 infection in persons who were routinely, heavily exposed to wild ducks and geese through recreational activities (duck hunting) or through their employment (bird banding).” In the realm of domestic birds, direct H7N7 infection of humans can lead to mild illnesses, such as conjunctivitis, and even to more serious disease (see here). Of particular note is the finding from the H11N9 study group of a “…relative lack of antibody response in our study population, who had substantial exposures to waterfowl with influenza A infections, and in inoculated volunteers from Beare and Webster (12) suggests that avian influenza infections in humans exposed to wild waterfowl may occur more commonly than we are able to detect with current methods.” Induction of mere low antibody responses, if coupled to high rates of adaptation to mammalian hosts with high pathogenicity characteristics, is a worrisome combination for human health.
 A Newly Confirmed Case of Flu A/H7N9 in Shanghai
A Newly Confirmed Case of Flu A/H7N9 in Shanghai
04Jan14
The official Chinese news agency, Xinhua, is reporting online yet another confirmed case of human H7N9 infection, this time in the city of Shanghai. The patient (86M) was confirmed with H7N9 yesterday and is currently hospitalized for treatment. No other details are currently available. this latest case increase the number of confirmed cases this season to 14 with one fatality. Since the onset of human H7N9 infections last spring, 149 confirmed cases have been reported with 46 fatalities.
In the bubbling cauldron of influenza strains currently percolating in South Asia, a new dimension has emerged. Reports (see here and here) have emerged of a new outbreak of avian H5N1 in southwestern China and in India. More fodder for potential influenza recombinants.
 Confirmed Cases of H7N9 Swell to 182 in Advance of Lunar New Year Celebrations
Confirmed Cases of H7N9 Swell to 182 in Advance of Lunar New Year Celebrations
16Jan14
The global number of confirmed cases of human infection by influenza H7N9 has swollen to 189 with 54 fatalities. Twenty one newly confirmed cases and three additional fatalities have been reported since our last update on 11Jan14, although the identity of the latest fatality in Guangdong Province is not clear. Overall, 54 cases have been reported just this season including 7 fatalities. The latest stats and a breakdown of new cases by country & province can be found here. A table with details of confirmed H7N9 cases can be found here.
The vast majority of cases emanate from mainland China this season, as last. To date, 50 cases of human A/H7N9 infection have been reported from the mainland, three from Hong Kong, and 1 from Taiwan (ex Jiangsu Province on the mainland). The outbreak continues its geographic spread this past week, with the first (and fatal) infection reported from Guizhou Province in SW China. There were no confirmed cases of H7N9 infection from this province last season.
A cursory visual inspection of the case data this season seems to indicate a shift towards a younger demographic (compared to the outbreak last Spring). While season flus typically cause mortality in the very old and the very young, pandemic strains of influenza disproportionately effect the young and middle-aged adults. A genetic cause for a possible shift in the age range of affected patients is not currently evident.
Of the 21 new cases in the past 5 days, 9 were reported from Zhejiang Province and six were from Guangdong Province. Thus, the trend observed earlier in the season of two primary foci for the outbreak, one in northern China and the other in southern China appears to be holding.
In a special Insight piece, the official Chinese news agency Xinhua highlighted official concerns about the potential impact of the upcoming Spring Festival (Lunar New Year). "During the world' s biggest annual human migration in the 40 days around Spring Festival, about 3.62 billion trips will be made this year, according to Tuesday's National Development and Reform Commission press release." As a result, "The virus is more active in winter and spring, and high density transportation in coaches, trains and aircraft could create "favorable circumstances" for the epidemic to spread, according to Li Lanjuan of the Chinese Academy of Engineering."
Already, the number of new cases seems to be accelerating. Look for many more confirmed cases of H7N9 over the next weeks.
 An H5N1 Fatality in Canada
An H5N1 Fatality in Canada
10Jan14
The news was stunning. The first fatality in North America due to the highly pathogenic influenza virus H5N1 was reported from Alberta, Canada (see here, here, and here). The patient (female, late 20's) first showed symptoms on a flight from Beijing to Vancouver on Dec. 27th. She had been in China most of December with her mother on a family vacation. The patient was a registered nurse and went to hospital on 28Dec13 after returning to Edmonton with fever and headache. While she went home later in the day, she returned to the hospital on 01Jan14. Unfortunately, her condition worsened and she passed away on 03Jan14. Infection by H5N1 was confirmed on 08Jan14.
The case is also surprising for a couple of additional reasons. First, the patient spent all of her time in China in Beijing. She did not visit any farms or go to any markets. Moreover, there have been no reported human cases of H5N1 in Beijing (in fact, there are no reported human H5N1 cases in China since Feb13). Typically, human infection with H5N1 occurs after direct contact with infected poultry. Thus, exactly how the patient came to be infected is unclear.
Second, the patient's symptoms were reportedly atypical for H5N1 infection. There was neither cough nor respiratory symptoms. "Alberta’s chief medical health office has said the woman had neurological symptoms that made doctors suspect she had encephalitis, or a brain infection. It’s not a common symptom of flu but has been reported in some H5N1 cases."
As noted by Recombinomics, a similar atypical course with a primary diagnosis of gastrointestinal infection and acute encephalitis was described for two Vietnamese siblings in a 2005 article in the New England Journal of Medicine. These are common diagnoses in SE Asia and the further finding of live virus isolation from CNS fluid and rectal specimens.
The implications of the clinical presentation of the present Canadian case and the 2004 Vietnamese cases are of enormous potential import to public health responses (e.g. surveillance) as well as clinical diagnosis and treatment of H5N1.
 U.S. Flu Activity Takes a Slight Pause in Week 1
U.S. Flu Activity Takes a Slight Pause in Week 1
10Jan14
The latest data from the CDC for the week ending January 4th (week 1) has been published. The data shows that flu activity in the U.S. again is still robust, though some indicators were down slightly from the week prior (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 26.2% nationally, compared to 26.7% the prior week. Regions 5 [IL, IN, MI, MN, OH, WI], 6 [AR, LA, NM, OK, TX], 8 [CO, MT, ND, SD, UT, WY], and 10 [AK, ID, OR, WA] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). All other regions showed values above 20% but below the national average, save for Region 2 which came in at 17% of respiratory specimens positive for influenza.

The pneumonia and influenza (P&I) mortality index is 6.9% (6.5% last week), below the epidemic threshold of 7.1% for week 1, and there were four influenza-associated pediatric deaths reported: three that were ascribed to 2009 H1N1p and one ascribed to a not-subtyped influenza A. The proportion of outpatient visits ascribed to influenza (ILI) was 4.4% (versus 4.3% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows twenty states with “high ILI activity” (see table below) and 7 + NYC with "moderate ILI activity". When typed, the majority of isolates were influenza A (~97% of typed specimens) and, while only 57% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 99%; 0.4% were H3N2).
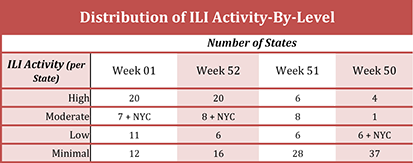
The number of Tamiflu-resistant isolates detected this season increased to 13, and the % of tested isolates found to be Tamiflu-resistant fell to 1.2% (from 1.1%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
Inspection of the recent data would suggest that influenza will resume its upward trend in the coming weeks. Many of the most populated regions of the country have yet to feel the full brunt of the flu and there is no reason to think they won't. Overall vaccination rates in the population are thought to be low (perhaps just 40% or so?) and, once seeded, it is difficult to stop the spread of flu in heavily populated areas. Although the flu season peaked last year at point, trends in the available data suggest we have some yet before a peak.
More concerning are the number of press reports emerging that tell of ICU's strained to the maximum and near peak utilization of available respirators/ECMO machines (see, for example, here and here). Another sign of stress in the system are the recent new stories of various states/provinces in the US and Canada running low on, and in one case out of, flu vaccine (see for example here, here, and here). While these stresses are all manageable, they do serve as a useful indicator of the current flu environment.
And there is persisting concern around the observation that so many of the hardest hit patients are the young and middle-aged adults, a patient demographic more typical of a pandemic influenza strain than a usual seasonal flu. A recent news report suggests that TX, having just gone the distance with influenza, is now battling an outbreak of severe RSV in the Houston area.
 U.S. Flu Activity Week 51 Update: A Pre-Holiday Rush
U.S. Flu Activity Week 51 Update: A Pre-Holiday Rush
27Dec13
The latest data from the CDC for the week ending December 21th (week 51) has been published. The data shows that flu activity in the U.S. again increased significantly over the preceding week (for a graphical round-up of the data, please see here). The percentage of respiratory specimens testing positive for influenza increased to 24.1% nationally, up from 17.8% the prior week. Regions 5 [IL, IN, MI, MN, OH, WI], 8 [CO, MT, ND, SD, UT, WY], and 10 [AK, ID, OR, WA] led the pack with a % of specimens positive for flu in excess of the national average (see graph, below). Regions 4 [AL, FL, GA, KY, MS, NC, SC, TN] and 6 [AR, LA, NM, OK, TX] followed, just below the national average at 22.6% and 23.1%, respectively, while the remaining regions were below the national average.
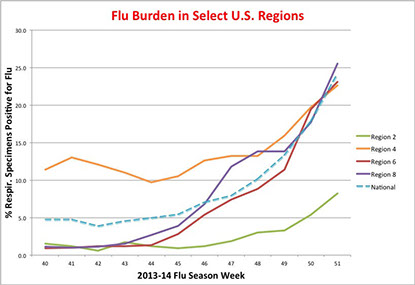
The pneumonia and influenza (P&I) mortality index is 6.7% (6.6% last week), below the epidemic threshold of 6.9% for week 51, and there was one influenza-associated pediatric death reported, ascribed to influenza B, that occurred last season. The proportion of outpatient visits ascribed to influenza (ILI) was 3% (versus 2.3% last week), again above the national baseline of 2%. The distribution of ILI activity-by-state now shows six states with “high ILI activity” (see table below) and 8 with "moderate ILI activity". When typed, the majority of isolates were influenza A (~98% of typed specimens) and, while only 58% of influenza A specimens were subtyped, the vast majority of these were identified as 2009 H1N1p (roughly 98%; roughly 2% were H3N2).

The number of Tamiflu-resistant isolates detected this season increased to 10 (up from 7), though the % of tested isolates found to be Tamiflu-resistant remained constant (at 1.3%). By comparison, the CDC identified two Tamiflu-resistant isolates during the entire 2012-2013 flu season.
This past week also saw a spate of reports that may suggest the current 2009 H1N1p is especially nasty, especially in Texas. In the Houston area, a total of 13 confirmed deaths from 2009 H1N1p infection have been tallied this season, the most recent fatality on Christmas day, according to a local news report. Other fatalities have been reported elsewhere in the state.
On Dec 24th, the CDC issued a HAN Advisory stating that "From November through December 2013, CDC has received a number of reports of severe respiratory illness among young and middle-aged adults, many of whom were infected with influenza A (H1N1) pdm09 (pH1N1) virus." As is typical for pandemic influenza viruses, those hardest hit are younger adults and teenagers. And it's not just TX that has been hard hit: other local news reports tell of 2009 H1N1p cases with more severe symptoms and even fatalities in TN, MO, and MN, for example. Recombinomics has suggested today that 2009 H1N1p variants associated with more severe disease and mortality (e.g. HA D225G and Q226R) may be circulating more widely (at least in some regions) than deposited sequence data would infer.
A combination of higher levels of Tamiflu-resistance and enhanced virulence in 2009H1N1p could be problematic; the prevalence of both of these characteristics in the circulating viral population warrants continued close scrutiny.
 Welcome to the Americas, Chikungunya!
Welcome to the Americas, Chikungunya!
18Dec13
The first-ever documented case of “local” chikungunya virus infection in humans in the Americas has been reported on the Caribbean island St. Martin according to a ProMED email. “As of 10 Dec 2013, altogether, 2 confirmed, 4 probable, and 20 suspected cases of chikungunya [virus] infection have been reported.” A more recent news report states that the number of confirmed cases is now “about a dozen” with “dozens more” suspected cases. The WHO and the U.S. CDC are both citing ten confirmed cases on the island. The U.S. CDC has issued an alert (Watch Level 1) for those traveling to St. Martin.
According to the CDC, “A total of 109 laboratory-confirmed cases of chikungunya were identified in the United States from 1995 through 2009. All were in travelers, and all but three of them occurred between 2006 and 2009 when there were large outbreaks of the disease ongoing in India and Indian Ocean Islands. From 2006 through 2009, an average of 26 travel-related chikungunya cases was identified per year.” Globally, chikungunya has re-emerged in 2004, after years of chemical spraying directed at its mosquito host, and has spread to new locations across the globe, including Europe. Annually, there are millions of cases in countries across the globe, but especially around the Indian Ocean.
Chikungunya is an acute febrile viral disease that is rarely fatal. Patients usually present with the onset of high fever, severe joint pain, and rash. The disease was first identified in Africa in the 1950’s on the Makonde Plateau. The name chikungunya is derived from the Makonde verb kungunyala, refering to “that which bends up”; patients with long-term joint pain in the lower extremities develop a stooped gait. Infection with chikungunya virus is rarely fatal but the joint pain (polyarthralgias) seen with chikungunya can often be severe and debilitating. There is currently neither vaccine nor therapeutic agent for the infection. Patients recover in about a week, although long-term joint pain occurs in some people.
The virus does not spread person to person. Like its closely related viral cousin, dengue, the virus is spread by mosquitoes, notably Aedes aegypti and Aedes albopictus. Both of these strains are seeping into the U.S. and this past season saw a number of dengue cases in the U.S., especially in Florida and Texas. As these mosquito vectors gain a better foothold in the U.S., the number of cases of mosquito-born viral diseases, such as dengue and chikungunya, are expected to grow.
© 2012-2014 Acton Biotech Consulting - See Image Credits page for attribution and license conditions for non-original images/media.
Important DISCLAIMER - This is a science & technology website and not a medical treatment or diagnostic site. No information contained within this site is a substitute for advice or direction given by qualified medical professionals, nor is it intended to inform patients regarding treatment options or disease diagnosis/prognosis. As always, individuals should consult their own medical team about issues concerning their health and well being.

